Prepatellar [in front of kneecap] Bursitis
last updated by Cory Calendine, MD, Orthopedic Surgeon
A bursa is a small, fluid-filled sac located throughout the body, including around the hip, knee, hip, shoulder, and elbow. Bursa normally contain a small amount of fluid and sit between bones and soft tissues to cushion and enable low-friction movement.
Prepatellar bursitis is inflammation of the bursa (fluid-filled sac) in the front of the patella (kneecap). When the bursa becomes irritated and inflamed, it produces excessive fluid causing swelling, joint fullness, and pain in the knee joint.
Causes of Prepatellar Bursitis
Prepatellar bursitis is often triggered by repetitive external pressure from kneeling. Manual laborers including plumbers, roofers, carpet layers, coal miners, and agriculture workers are at higher risk for developing the condition.
Prepatellar bursitis can also be caused by a direct blow to the front of the knee joint, putting many athletes at greater risk for the condition.
Additionally, some patients with preexisting inflammatory diseases (including rheumatoid arthritis and gout) are predisposed to prepatellar bursitis.

Less commonly, prepatellar bursitis can be caused by a bacterial infection of the bursa. Knee injuries which cause a break in the skin (cut, insect bite, puncture wound) can allow bacteria to invade the fluid-filled bursa in front of the kneecap. This condition is called infectious prepatellar bursitis and is a more serious condition, often requiring more emergent treatment.
Symptoms of Prepatellar Bursitis
- Pain with knee joint movement (less commonly at night)
- Rapid swelling just in front of the kneecap
- Tenderness and warmth to touch of the kneecap
[Bursitis caused by infection can produce joint redness and systemic fever and chills]
Diagnosis and Treatment of Prepatellar Bursitis
- X-rays: provide clear pictures of bone and soft tissue and assist to rule-out other causes of anterior knee pain and swelling
- Other Imaging: computerized tomography (CT) and magnetic resonance imaging (MRI) scans may be ordered (less commonly) to provide a more detailed view of the joint and soft tissue
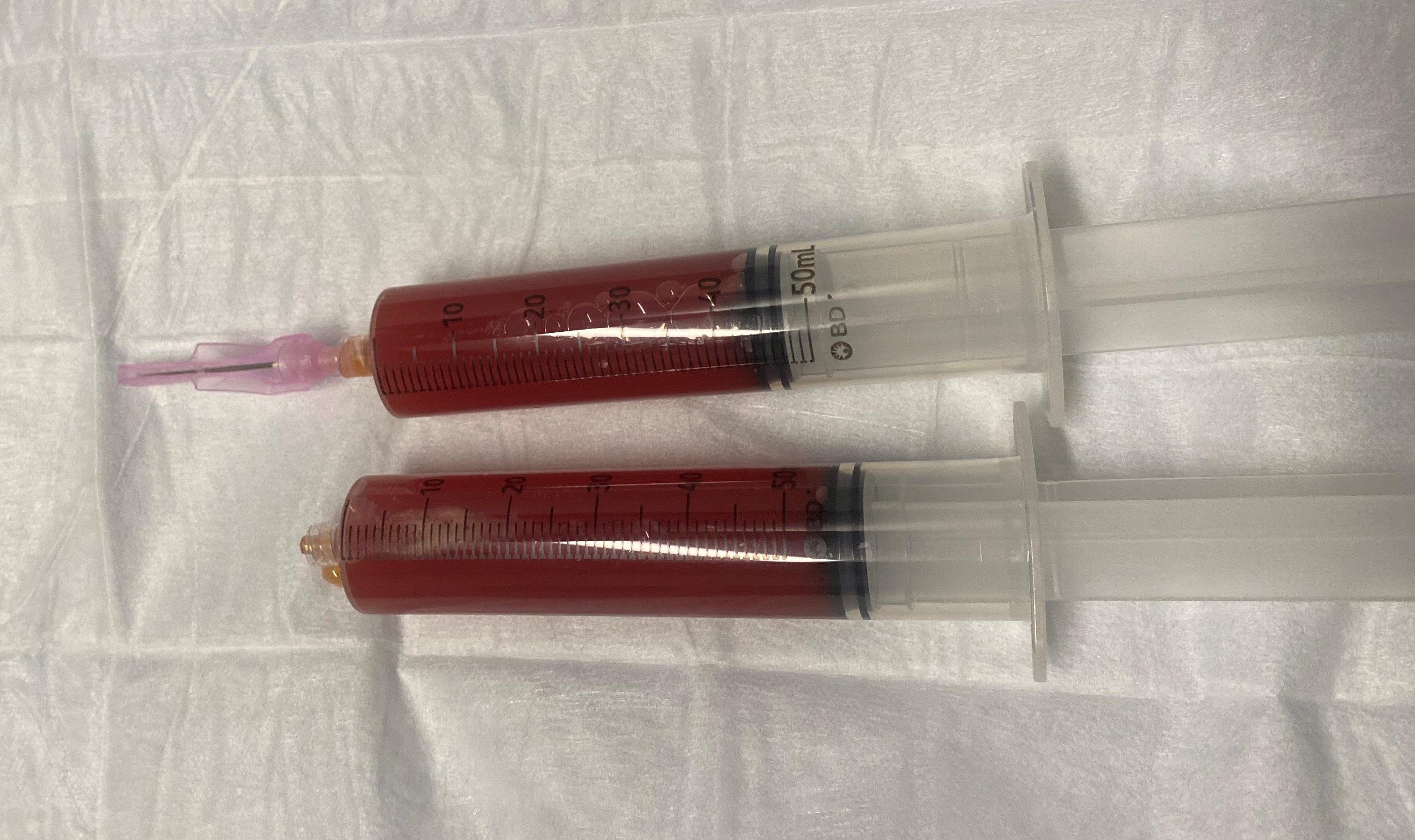
- Aspiration: Withdrawing excess fluid from the bursa can be both diagnostic and therapeutic. If recommended, Dr. Calendine can complete aspiration of the bursa fluid at your office visit. While draining fluid can reduce pressure on the joint, the fluid can be sent for laboratory analysis to help rule out joint infection.
Conservative (nonsurgical) Treatment
- Avoid the activities that apply pressure to the knee joint (while still remaining active).
- Apply ice at regular intervals 3 or 4 times a day for 20 minutes at a time to reduce swelling
- Elevate the affected leg except when possible to help limit swelling.
- Nonsteroidal anti-inflammatory drugs (NSAIDs) medications (such as naproxen and ibuprofen) may be recommended to help relieve pain and control inflammation.
Aspiration of Fluid
If the swelling and pain do not improve with more conservative measures, Dr. Calendine may choose to drain (aspirate) the bursa with a needle and sometimes then inject the bursa with a corticosteroid (to limit further inflammation). Bursa aspiration can be completed in the outpatient office with minimal discomfort.
Infectious Prepatellar Bursa
Infectious bursitis is more dangerous condition and requires is initial treatment with antibiotics. Surgical drainage may be required if the infection does not respond to antibiotics alone.
More information about Infectious Prepatellar Bursitis from AAOS CLICK HERE
RELATED ARTICLES