

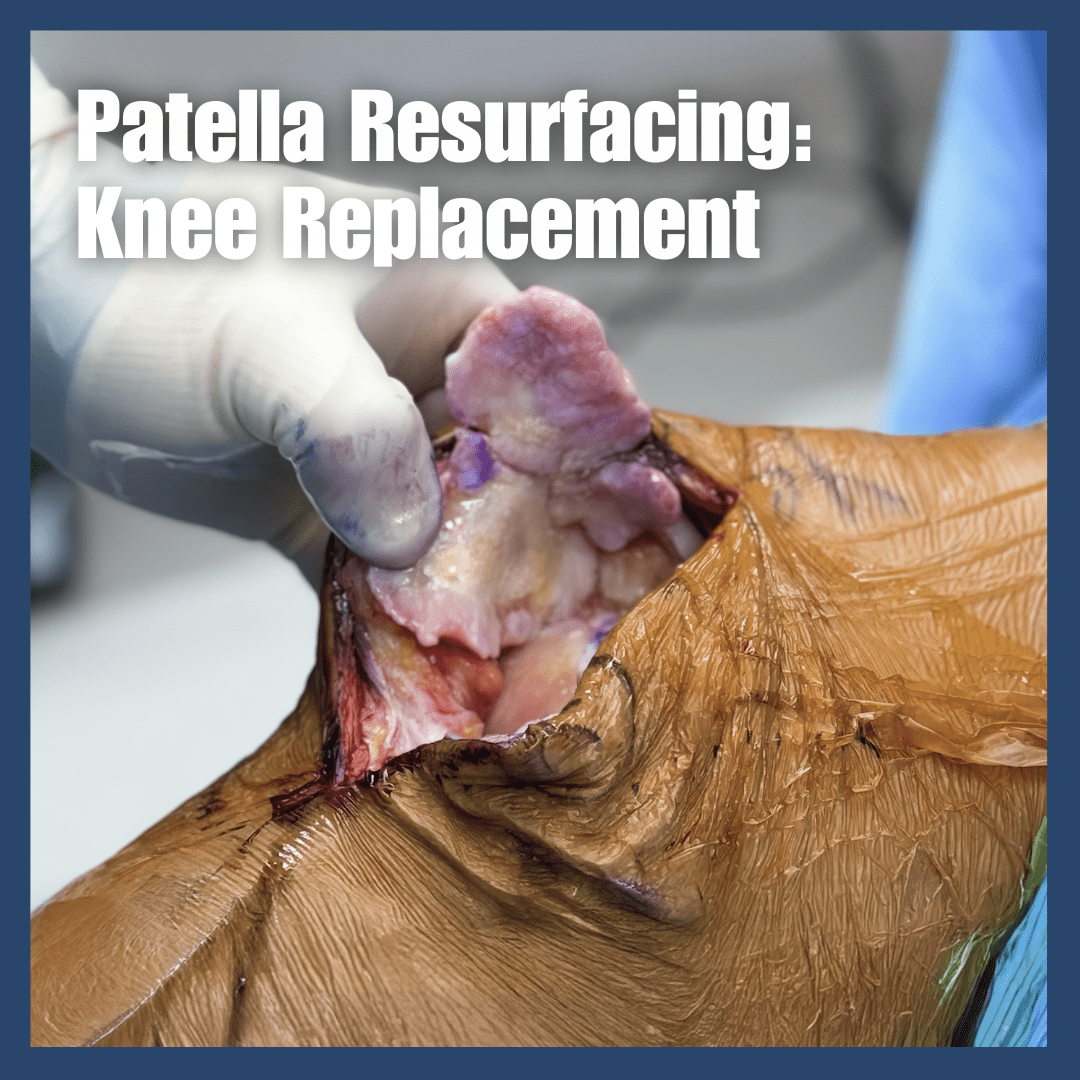
Patellar resurfacing is a critical decision during total knee replacement surgery where the damaged cartilage on the back of your kneecap is removed and replaced with a plastic component, or left in its natural state. This comprehensive guide explains how orthopedic surgeons decide whether to resurface the patella based on factors including cartilage damage severity, bone thickness, arthritis type, and patient-specific considerations. Patients in Franklin, Brentwood, and the greater Nashville area seeking knee replacement surgery will learn about the benefits and risks of both patellar resurfacing and non-resurfacing approaches, surgical techniques used, recovery expectations, and how modern knee implants have made both options viable for achieving pain relief and improved function. Whether you're experiencing anterior knee pain from patellofemoral arthritis or considering total knee arthroplasty, understanding patellar management options helps you have informed discussions with your orthopedic surgeon about the best approach for your individual needs and anatomy.
Read More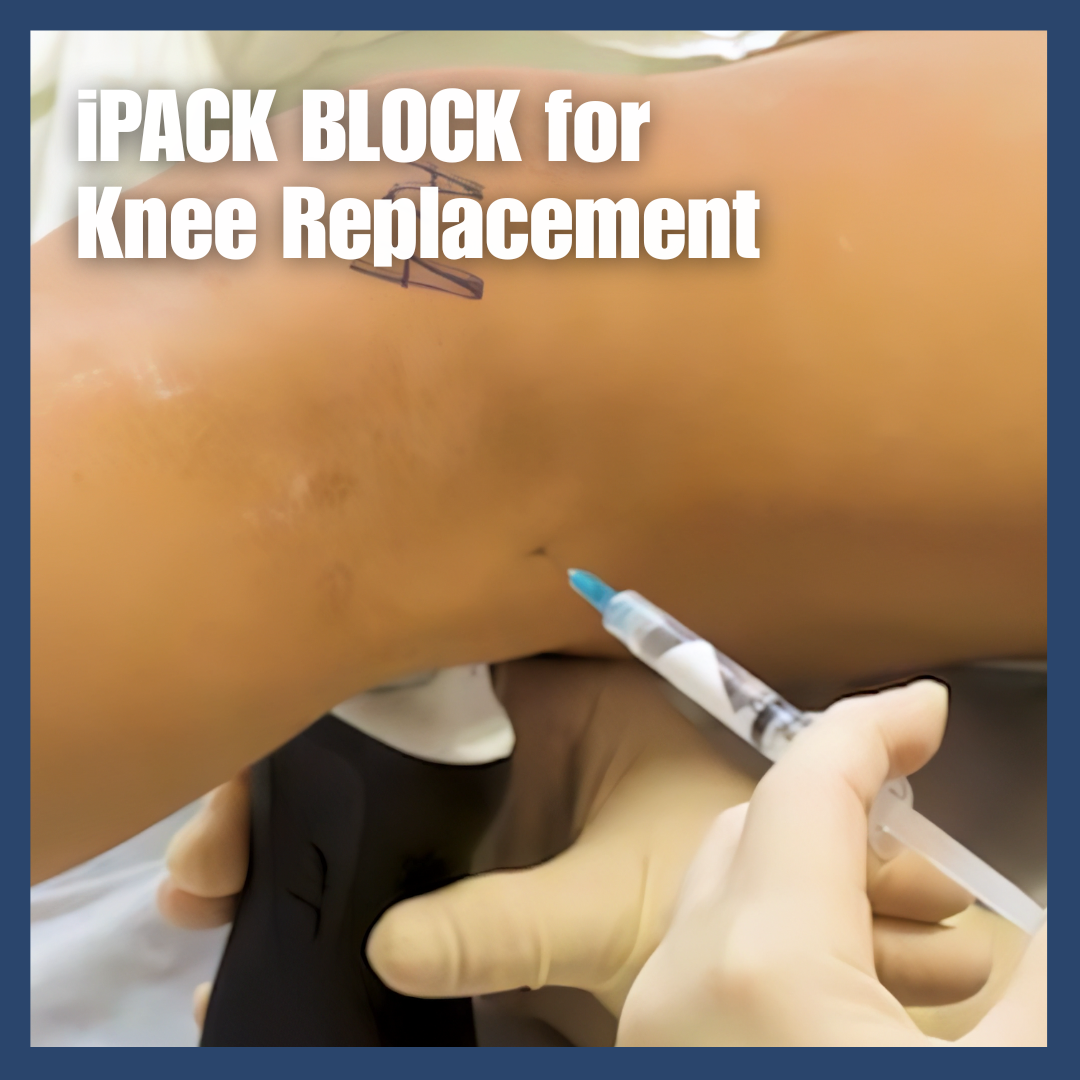
The iPACK nerve block is an advanced pain management technique that provides superior pain relief for knee replacement patients by targeting the posterior aspect of the knee joint that traditional nerve blocks miss. When combined with adductor canal blocks, this ultrasound-guided procedure reduces opioid requirements by up to 30% and enables faster recovery without affecting muscle strength. Dr. Calendine utilizes this evidence-based approach to help patients achieve better pain control and accelerated rehabilitation following total knee arthroplasty.
Read More
Discover if you're a candidate for subvastus robotic-assisted knee replacement – a muscle-sparing technique available to 90-95% of knee replacement patients. This advanced approach preserves your quadriceps muscle, leading to faster recovery, less pain, and quicker return to daily activities. Learn about candidacy requirements, expected outcomes, and why patients walk within days instead of weeks. Dr. Cory Calendine explains who qualifies for this revolutionary knee replacement technique and how robotic precision enhances results for active adults in Franklin and greater Nashville.
Read More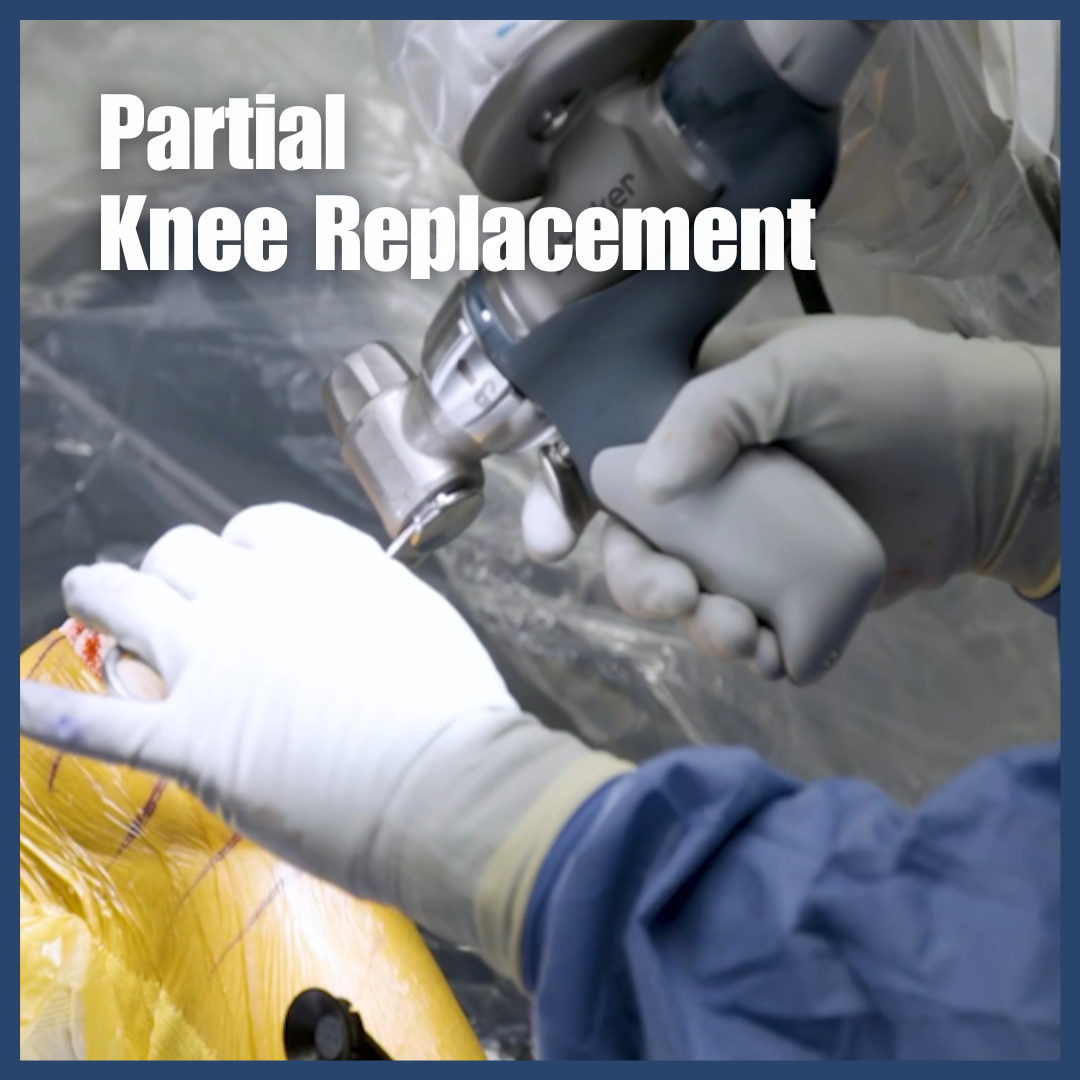
Partial knee replacement, also known as unicompartmental knee arthroplasty, offers a less invasive alternative to total knee replacement for patients with arthritis confined to one compartment of the knee. This minimally invasive procedure uses a 3-4 inch incision compared to the 7-8 inches required for total replacement, resulting in faster recovery times, shorter hospital stays (1-2 days vs. 3-5 days), and patients walking unassisted within 1-2 weeks. With over 90% success rates at 10 years and the ability to preserve healthy cartilage and natural ligaments, partial knee replacement provides excellent long-term outcomes for properly selected candidates. Learn about the surgical process, ideal patient characteristics, recovery timeline, and how this targeted approach can help you return to normal activities with minimal disruption.
Read More.jpg)
Learn the key differences between subvastus and medial parapatellar knee replacement approaches from Dr. Cory Calendine in Franklin, TN. Discover why the muscle-sparing subvastus technique combined with Mako robotic technology offers faster recovery than traditional methods. Get the facts about Jiffy Knee marketing claims versus proven surgical techniques, and understand how quadriceps-sparing surgery reduces pain and accelerates healing for Nashville area patients seeking advanced knee replacement options.
Read More
Discover the subvastus approach to knee replacement combined with Mako robotic technology for faster recovery and less pain. Dr. Cory Calendine explains how this muscle-sparing, minimally invasive technique preserves your quadriceps muscle, reduces surgical trauma, and gets you back to your active lifestyle quicker than traditional methods. Learn why robotic-assisted SubV knee replacement is revolutionizing orthopedic surgery in Franklin, TN and greater Nashville.
Read More
PRP injections for knee arthritis offer a promising alternative for patients seeking relief without surgery, using your body's own healing mechanisms to reduce pain and inflammation. This comprehensive guide explains how platelet-rich plasma therapy works, what to expect during treatment, and why many patients experience 6-12 months of improved function and pain relief. Learn about the science behind PRP, success rates showing 60-70% of patients benefit, how it compares to steroid injections and other treatments, and whether you're a good candidate for this innovative approach. With proper recovery support and realistic expectations, PRP therapy can help you return to activities you love while potentially delaying or avoiding knee replacement surgery.
Read More
Total knee replacement surgery involves minimal bone removal, with surgeons removing only 5-10 millimeters of damaged bone from the joint surfaces of the femur, tibia, and patella. This conservative approach preserves healthy bone while creating space for artificial components made of metal and plastic. The procedure is more accurately described as surface replacement rather than total bone removal, as advanced surgical techniques ensure only damaged cartilage and minimal bone are taken away. Factors determining bone removal include joint damage severity, implant type, and patient bone density, while benefits of controlled bone removal include enhanced prosthetic fit, preserved bone health, and better recovery outcomes. Modern knee replacement surgery provides excellent long-term results with implants lasting 15-20 years, restored mobility, and significant pain relief for patients suffering from arthritis and other degenerative joint conditions.
Read More
During total knee replacement surgery, orthopedic surgeons strategically manage knee ligaments to optimize implant placement and long-term stability: the anterior cruciate ligament (ACL) is routinely removed due to pre-existing arthritis damage and to allow proper implant positioning, while the medial patellofemoral ligament (MPFL) is typically released but may be repaired or reconstructed if patellar instability is present. The posterior cruciate ligament (PCL) fate depends on implant design - it's preserved in cruciate-retaining implants but removed in posterior-stabilized designs, with both approaches showing similar long-term outcomes. The medial and lateral collateral ligaments are carefully preserved and balanced during surgery to maintain essential side-to-side knee stability, while the menisci are removed and replaced by the implant's plastic spacer component, ensuring patients receive optimal biomechanics and stability from their total knee arthroplasty procedure.
Read More
Tylenol (acetaminophen) and Ibuprofen are both common over-the-counter medications frequently used to treat arthritis pain. Tylenol and ibuprofen are not the same types of medication. While Tylenol is a non-aspirin pain killer, ibuprofen is a member of the non-steroidal anti-inflammatory medication class (NSAIDs). There are risks and side effects to be considered and proper dosage is important to help avoid medication complications.
Read More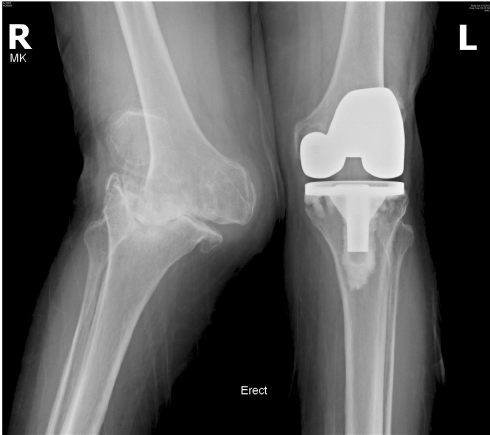
Knee replacement is an advanced orthopedic procedure that has helped thousands of people regain movements and experience dramatic pain relief. Arthritis is a leading cause of pain and disability. When should you consider knee replacement surgery? Are you a good candidate for knee arthroplasty? Dr. Cory Calendine, an orthopaedic surgeon in the Nashville region, explains the benefits and limitations when considering knee replacement surgery.
Read More
Dr. Cory Calendine, Orthpaedic Surgeon, discusses the most common mistakes for knee replacement patients to avoid. From having a postoperative care plan to taking pain medications appropriately, avoiding these knee replacement mistakes is vital to optimize joint replacement recovery and ultimate outcomes.
Read More
Hip and Knee Replacement surgery complications have shown to be higher in patients with a body mass index [BMI] that is too high or too low. Maintaining a healthy BMI can decrease complications of joint replacement surgery and improve postoperative recovery.
Read More
Prepatellar bursitis causes swelling, stiffness and pain of the anterior knee joint. The condition is often triggered by repetitive pressure or injury to the anterior knee. Although conservative treatment is often useful, joint aspiration can provide symptoms relief and help better diagnose the cause of knee inflammation.
Read More
Hip and knee replacement surgeries have seen significant advancements over the last 20 years. Many procedures today are so effective that, as Cory Calendine, MD, Orthopaedic Surgeon at Bone and Joint Institute of Tennessee reports, “The biggest patient complaint I get after joint replacement is: ‘Why didn’t I do that earlier?’” Read more about advances in hip and knee replacement including robotics, advanced surgical techniques and outpatient surgery options.
Read More
Robotics are increasing being used by Orthopaedic Surgeon as a tool to help optimize joint replacement planning and execution and improve patient outcomes. During the 4th Annual Joint Replacement Awareness Day, Cory Calendine, MD presented a brief introduction to Robotic-Assisted Joint Replacement.
Read More.png)
Cory Calendine, MD outlines the process and advantage of MAKO Robotic-Assisted Knee Replacement and walks you through the steps involved in a robotic-assisted total knee replacement surgery. Robotics are used in joint replacement procedures to improve accuracy, precision and patient outcomes.
Read More.png)
Artificial Intelligence may offer decision-making assistance for patients dealing with joint osteoarthritis. New medical research has demonstrated that artificial intelligence augmented treatment decision tools offer benefits over more traditional digital patient education materials.
Read More%20Resurfacing%2C%20CORY%20CALENDINE%2C%20MD.png)
Ever wonder what happens to the kneecap (patella) during knee replacement? The decision to resurface the underside of the patella as part of total knee replacement may be influenced by a number of factors. Dr. Cory Calendine, Orthopaedic Surgeon discusses the process of patella resurfacing during knee replacement surgery.
Read More
Advanced surgical techniques and pain control methods allow most joint replacement patients to begin ambulating and moving immediately after surgery with few limitations. Many hip and knee replacement patients return to normal daily activities within 4-6 weeks. Physical therapy and follow-up is customized for each patient's individual recovery journey.
Read More
Both heat and cold therapy are utilized by patients in attempts to relieve joint pain and stiffness. Dr. Cory Calendine, Nashville Orthopaedic Surgeon discusses the differences, benefits and uses of both hot and cold therapy for bone and joint pain and stiffness.
Read More.png)
Do your hips and knees feel stiff when you wake up in the morning or after sitting for a period of time? There are several reasons why prolonged inactivity may cause joint stiffness and pain. From home treatments to surgical intervention, Dr. Cory Calendine discusses 13 ways to find relief from stiff joints.
Read More.png)
Meniscus tear is one of the most common knee joint injuries. This article explains the anatomy of knee menisci, mechanism of injury and symptoms and treatment following a knee meniscus tear. Treatment of meniscus injury can differ when associated with knee joint arthritis.
Read More.png)
Surgery to replace a hip or knee joint is complex, lasts about an hour to an hour and a half, and comes with some potential complications. A rare complication following knee or hip replacement is the development of a blood clot or deep vein thrombosis. A medication called Warfarin (previously used as a rat poison) is used along with other treatments to prevent blood clots after joint replacement surgery.
Read More.png)
A major concern of many patients considering joint replacement surgery is how painful is it? Advanced pain control techniques and methods have made joint replacement surgery a less painful procedure over the past several years. Improved pain control methods allow much less use of narcotic medications and permit most patients to return home much sooner after hip or knee replacement surgery.
Read More
During total knee replacement, orthopaedic surgeons will often resurface the articular surface of the kneecap. Cory Calendine, MD, Orthopaedic Surgeon discusses patella resurfacing during total knee arthroplasty and how the procedure resembles an Oreo cookie.
Read More.png)
There is a link between weight gain, obesity, and osteoarthritis. A high body weight or body mass index (BMI) can put additional pressure on your knees, increase inflammation and increase your risk of joint damage and pain. Taking the necessary steps to manage your weight can help protect your knees from joint pain and reduce your risk of osteoarthritis. Start a path to joint pain freedom with nutritious eating, increased activity and weight loss.
Read More