Mental Health and Chronic Pain
Both depression and generally poorer mental well-being are more prevalent among individuals dealing with chronic pain. Additionally, poorer mental health is consistently associated with reduced overall health-related quality of life and even poorer outcomes of medical and surgical treatments.
Osteoarthritis and Mental Health
Osteoarthritis is one of the most prevalent chronic pain conditions globally and is a leading cause of disability. The prominent symptom of osteoarthritis, and leading factor for seeking medical care and surgical intervention, is pain. Chronic pain is a strong predictor of clinical depression in osteoarthritis patients and contributes to patient-reported disability associated with chronic osteoarthritis joint pain.
Researchers once thought the relationship between pain, anxiety, and depression resulted mainly from psychological rather than biological factors. Chronic pain is depressing, and likewise major depression may feel physically painful. But as researchers have learned more about how the brain works, and how the nervous system interacts with other parts of the body, they have discovered that pain shares some biological mechanisms with anxiety and depression. Treatment is challenging when pain overlaps with anxiety or depression.
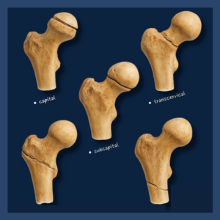
Studies consistently find that poor mental health is reported among patients with pain and functional disability and is common in osteoarthritis patients. Osteoarthritis and mental health disorders are leading causes of disability in older adults. Depressive symptoms in people with hip osteoarthritis are higher (23–34%) compared with other chronic diseases such as diabetes, coronary heart disease or cancer (16–24%). More specifically, depressive symptoms were found in 34% of OA patients on a waiting list for total hip arthroplasty (THA), and in 23% of patients waiting for total knee arthroplasty (TKA). With the relationship among pain, disability and mental health, should the improvement in pain and function from total joint arthroplasty (or replacement) also result in improvement in mental health?
Total Hip Replacement and Mental Health
New research attempts to examine the relationship between degree of pain and function improvement and mental health improvement after THA – and the results are encouraging. Mental health improved from baseline to 1-year following THA. The degree of improvement in mental health strongly correlated with the degree of improvement in pain and function (taking into account additional potential factors).
Patients considering total joint replacement, should consider that improvement in mental health can be an important benefit of surgical intervention. Depression or mental health stress frequently seen in patients with joint pain from osteoarthritis can be successfully improved with joint replacement surgery.
Tips for Coping with the Mental Effects of Chronic Pain
- Speak with your physician or other healthcare provider about symptoms of depression and/or anxiety
- Educate yourself about your condition to reduce fear of the unknown.
- Consider meditation and mindfulness practices
- Exercise (as much as you are able and with your physician's guidance)
- Consider seeing a mental health counselor for talk therapy.
- Some people might need medication to treat insomnia, depression, or anxiety.
- Do not fall into self-medication! Using substances might temporarily alleviate physical or emotional pain, but this is never a good long-term solution.
If you are continuing to deal with the consequences of chronic pain despite conservative therapy, contact Dr. Calendine today to discuss additional joint pain treatment options that my be best for you.