Subvastus vs Medial Parapatellar Knee Replacement: What Patients Should Know About Jiffy, Robotics, and Recovery
Patients today are more informed - and sometimes more confused - than ever. That is especially true when it comes to the different techniques used in knee replacement surgery. Terms like subvastus, medial parapatellar, and Jiffy Knee are everywhere online, but it is hard to know what really matters.
Let me clear it up.
This article explains the difference between the subvastus approach and the traditional medial parapatellar approach, why the subvastus (or "SubV") method may lead to faster recovery, and how robotics like the Mako system enhance precision and patient outcomes.
First, Let's Define the Two Main Surgical Approaches
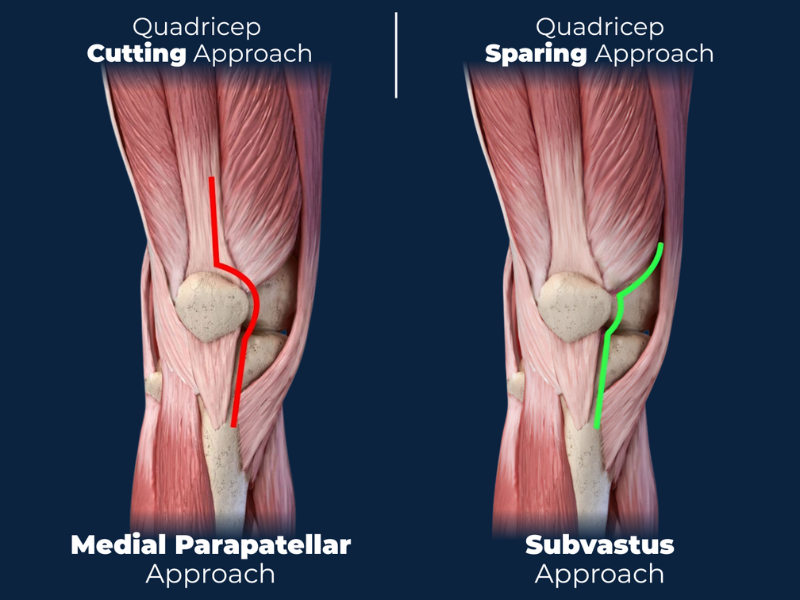
Medial Parapatellar Approach
This is the most commonly used approach in traditional total knee replacement. The incision goes through the quadriceps tendon and reflects the kneecap to access the joint. It provides excellent visibility for the surgeon but also involves:
- Cutting through the quadriceps tendon
- More trauma to surrounding soft tissue
- Longer time to regain normal walking and stair climbing
Subvastus Approach (SubV)
This technique avoids cutting the quadriceps tendon. Instead, the surgeon works underneath the vastus medialis muscle—hence the term subvastus.
What that means:
- No cutting of the quadriceps tendon
- Muscle-sparing, or quadriceps-sparing
- Potential for less pain and faster early recovery
This is the technique I use in most cases—especially when I can combine it with robotic-assisted precision using the Mako system.
What About the Jiffy Knee? Is That the Same as Subvastus?
Jiffy Knee® is a registered trademark of its respective owner. All references are made for informational and comparative purposes only.
Here is the thing: The Jiffy Knee is a trademarked term, not a surgical technique. According to their public website, the Jiffy Knee uses the subvastus approach. That is accurate—but the name itself is proprietary marketing.
I want to be clear:
I do not perform the Jiffy Knee. I perform a subvastus (SubV) approach, which is used by the Jiffy Knee per online sources, but also use robotics for further soft tissue protection, less trauma, more precision and promising an even faster recovery with less pain.
What I know about the Jiffy Knee is based on:
- Publicly available information on their website
- Conversations with other surgeons familiar with the term
At the time of writing, there are no scientific papers published on the "Jiffy Knee."
Science and Trust: Subvastus + Robotics Is a Proven Combination
While "Jiffy Knee" is a marketing term, subvastus total knee arthroplasty (TKA) is a well-studied and increasingly supported approach in the published medical literature.
Likewise, robotic systems like Mako have been shown to improve implant precision, reduce soft tissue damage, and lead to more predictable outcomes.
In fact, a new study published in the Journal of Clinical Orthopaedics and Trauma (Sept 2025) confirms the benefits of combining subvastus technique with robotic technology.
This is the approach I trust—and the one I perform.
Other Names Patients Might See for the Subvastus Approach
Here's where the confusion often grows. The subvastus approach can go by several names, especially when practices or surgeons market their own brand of minimally invasive surgery.
Terms you might hear include:
- SubV Knee
- SubVy Knee
- Subvi Knee
- Suby Knee
- Suvi Knee
Which do you like the best?
These are not different techniques. They are alternative names used to describe the same underlying method: accessing the knee joint without cutting the quadriceps tendon.
If you are trying to compare options, focus less on the brand name and more on these questions:
- Will my quadriceps tendon be preserved?
- Is this truly a subvastus or muscle-sparing technique?
- Is the procedure assisted with robotic guidance like the Mako system?
So, Why Do I Prefer Subvastus with Robotics?
Simple. I believe in surgical methods that are:
- Backed by data
- Proven in peer-reviewed journals
- Designed to reduce pain, swelling, and time on crutches
- Enable patients to walk sooner and recover faster
Combining the subvastus approach with Mako robotic assistance helps ensure the implant is placed precisely, with minimal disruption to soft tissues.
The result? Patients who are walking comfortably in days—not weeks—and getting back to normal life faster.
How to Know If You Are a Candidate
Most patients with arthritis-related joint damage are strong candidates for this approach. It may not be appropriate for everyone—for example, patients with very tight tissue or complex deformities may need a traditional approach.
That is why I assess each patient individually using:
- Imaging
- Strength and flexibility exams
- Health history
- Goals for post-surgery activity
Let's Talk: Franklin, Brentwood, and Middle Tennessee Patients Welcome. If you are considering knee replacement and want to know if the SubV approach with robotics is right for you, I invite you to schedule a personal consultation. You will walk away with:
- A clear explanation of your options
- Honest answers to your questions about recovery
- A personalized surgical plan backed by science, not marketing
By Cory Calendine, M.D., Hip and Knee Replacement Specialist, Franklin, TN
*What I know about the Jiffy knee is from public (online) sources and personal communication with other surgeons. There are no scientific papers on the "Jiffy knee". There are many scientific papers on the benefits of the subvastus knee and robotics. Trusted, scientific literature combining these two proven methods - the subV approach and robotics - are now being published. I perform robotic subvastus total knee replacements at our surgical center in Franklin, TN and care for patients across Brentwood, Nashville, Spring Hill, and surrounding areas. If you are searching for a knee replacement expert in Tennessee who uses advanced techniques like SubV with Mako, I would be happy to discuss your options in a personal consultation.





a.png)


