Revolutionary Bone Glue Gun: A New Way to Fix Broken Bones
Scientists have developed a portable "bone glue gun" that can print biodegradable material directly into broken bones during surgery. This handheld device melts and shapes a bone-like composite on the spot, potentially eliminating the need for pre-made implants. Early studies show it promotes natural bone growth while providing immediate structural support.
What Is the Bone Glue Gun Technique?
Imagine walking into surgery with a broken bone and walking out with a custom-fitted repair, all done in one procedure. That's the promise of this new technology. The bone glue gun works like the craft glue guns you might have at home, but it's designed for the operating room. It heats a special stick made of bone-friendly materials and extrudes it directly into the fracture site. The surgeon can shape it in real-time to fit the exact contours of your bone. This isn't science fiction. Researchers recently published results showing this approach works in animal studies, and the implications for human patients could be significant.

How the Device Actually Works
The device uses two main ingredients: polycaprolactone (PCL) and hydroxyapatite (HA). Don't worry about pronouncing those - just know that PCL is a biodegradable plastic that gradually breaks down in your body, while HA is a mineral that makes up most of your natural bone. When heated to about 80°C (176°F), these materials melt and can be printed through different sized nozzles. The surgeon controls the flow, kind of like decorating a cake, but with bone-repair material. Here's what makes this different from traditional bone grafts: the material cools quickly once applied, hardens within seconds, and starts encouraging your own bone cells to grow almost immediately.
Why Traditional Bone Repair Has Limitations
I've treated hundreds of patients with fractures over the years. The current options work, but they're far from perfect.
Bone grafts require taking bone from another part of your body (usually your hip) or using donor bone. This means extra surgery sites, more pain, and potential complications. Plus, your body doesn't always accept grafted bone well.
Metal plates and screws provide great stability but stay in your body permanently unless removed in a second surgery. They can cause discomfort, set off metal detectors, and don't naturally integrate with your bone tissue.
Pre-fabricated implants come in standard sizes. Your bones, however, are unique. Getting a good fit often means settling for "close enough" rather than perfect.
The Gap This New Technology Fills
Large bone defects, gaps bigger than about an inch, don't heal on their own. Your body simply can't bridge that distance naturally. Until now, treating these defects meant choosing between imperfect options. The bone glue gun addresses several problems at once. It creates custom shapes, uses materials your body can absorb, and includes components that actively encourage bone regeneration.
What Makes This Technique Promising
The research shows some genuinely exciting results that caught my attention as an orthopedic specialist.
It Promotes Natural Bone Growth
The hydroxyapatite component acts like a magnet for your bone-forming cells. In laboratory studies, cells grown on this material showed increased production of proteins associated with healthy bone formation. Think of it as laying down scaffolding that your body recognizes and says, "Oh, I need to fill this in with bone." Over time, as the biodegradable material breaks down, your natural bone replaces it.
Customizable for Different Injuries
Not all fractures are the same. A crushed ankle bone needs different treatment than a simple arm break. The beauty of this system is its flexibility. Surgeons can adjust the material composition for different needs. More hydroxyapatite means stronger initial structure. Different molecular weights of PCL control how fast the material breaks down. The nozzle size determines how thick the extruded material is.
Built-In Infection Prevention
Here's something that really impressed me: the material can incorporate antibiotics directly into the mix. Bone infections after surgery are serious complications that can require months of treatment. With antibiotics embedded in the repair material, you get targeted, sustained release right where it's needed most. The studies showed this approach effectively prevented bacterial growth without the side effects of systemic antibiotics.
How the Procedure Would Work for Patients
Let's walk through what this might look like in practice. You'd come in for surgery as usual—under anesthesia, the surgical team would clean and prepare the fracture site. Here's where things differ from traditional approaches.
During Surgery
Instead of waiting for a pre-fabricated implant or harvesting your own bone, the surgeon would use the handheld device to print material directly into your bone defect. They'd shape it to match your anatomy exactly, filling gaps and providing immediate stability. The material cools to body temperature within about 40 seconds. That's fast enough to keep surgery time reasonable but slow enough to give the surgeon control over the final shape. Once the repair material is in place, the surgeon would use plates and screws for additional stability, just like with current methods. The difference is the bone-repair material itself fits perfectly.
Recovery and Healing
Your body would start the healing process immediately. The hydroxyapatite surface attracts bone-building cells. Blood vessels grow into the scaffold. Gradually, your natural bone replaces the temporary material. Recovery time would likely be similar to current procedures, you'd follow standard protocols for weight-bearing and physical therapy. The big difference happens inside: instead of living with permanent hardware or waiting for grafts to incorporate, you'd be growing your own bone back.
What the Research Actually Shows
The study published in September 2025 tested this technology in rabbits with large bone defects. Here's what they found. Animals treated with the bone glue gun material showed significantly better bone formation compared to traditional bone cement. Scans after 12 weeks revealed more new bone growth, better bone density, and improved structural integrity. The biodegradable implants maintained mechanical strength during the critical healing period, then gradually broke down as natural bone replaced them. No animals showed signs of rejection or adverse reactions to the material. These are animal studies, which means we need to be cautious about translating results to humans. But the findings are promising enough to warrant further investigation.

Potential Benefits for Different Types of Injuries
This technology could help with several challenging orthopedic problems.
Complex Fractures
When bones shatter into multiple pieces, reconstructing them is like doing a jigsaw puzzle—except some pieces are missing. The bone glue gun could fill those gaps while holding everything in position.
Bone Tumors
After removing a bone tumor, surgeons face a large defect that needs filling. Current options include large grafts or permanent metal implants. A biodegradable solution that promotes natural bone regeneration could be transformative.
Non-Healing Fractures
Some fractures just won't heal on their own, no matter how long you wait. These non-unions often need surgical intervention. The bone-stimulating properties of this material might give these stubborn fractures the boost they need.
Revision Surgeries
When previous bone repairs fail, revision surgery is more complicated. The bone glue gun's ability to conform to irregular shapes and damaged bone could make these difficult procedures more manageable.
What Still Needs to Be Answered
As promising as this technology is, we're still in the early stages. Several important questions remain. Will it work as well in humans as it does in animals? Human bones are larger, experience different mechanical loads, and have different healing rates. We'll need human trials to know for sure. How long does the material actually last? The studies showed it maintaining strength for 12 weeks, but some fractures need support for longer. More research will determine the optimal breakdown rate for different applications. What's the learning curve for surgeons? Any new technique requires training. We'll need to understand how much practice surgeons need to become proficient with this tool.
The Bigger Picture of Bone Repair Innovation
This bone glue gun represents a broader trend in orthopedics toward personalized, biologically-integrated treatments. We're moving away from one-size-fits-all solutions and toward repairs that work with your body rather than just sitting in it. Other technologies, like 3D-printed implants and growth factor therapies, are part of this same evolution. The goal isn't just to fix broken bones—it's to restore them to their natural state. Every step toward that goal improves outcomes for patients.
What This Means for You
If you're dealing with a fracture or bone defect right now, this technology isn't available yet for routine use. It's still in the research phase. But knowing what's in development can help you have informed conversations with your orthopedic surgeon about current treatment options and what might be available in the future.
Questions to Ask Your Doctor
When discussing treatment options for a fracture, consider asking:
- What are all my options for bone repair?
- How well does each option match my specific injury?
- What's the expected healing timeline?
- Will I need additional surgeries to remove hardware?
- Are there any clinical trials I might qualify for?
Looking Ahead
The bone glue gun technique is one of several promising advances in orthopedic care. While it may take years before it becomes standard practice, the research shows genuine potential to improve how we treat bone injuries. Medical technology moves forward through exactly this kind of innovation—taking a simple idea (what if we could print bone material directly into fractures?) and developing it into something that might genuinely help patients heal better. If you're dealing with a difficult fracture or bone defect, don't lose hope. Medicine is advancing, and your orthopedic surgeon has more tools and options than ever before to help you heal.
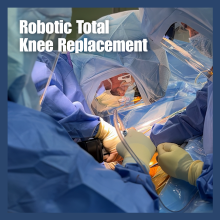
Expert Knee Replacement Care in Brentwood
Dr. Cory Calendine specializes in advanced orthopedic care, including complex knee replacements and fracture management, right here in Brentwood, Tennessee. With years of experience treating patients from across the greater Nashville area, Dr. Calendine stays current with the latest advances in orthopedic surgery while providing personalized, compassionate care. Whether you're dealing with arthritis requiring knee replacement, a complex fracture, or another orthopedic concern, our practice offers comprehensive treatment options tailored to your specific needs. We serve patients throughout Williamson County and surrounding communities, providing accessible, expert orthopedic care close to home.
To schedule a consultation with Dr. Calendine or learn more about your treatment options, visit www.corycalendinemd.com or call our Brentwood office today.
Medical Disclaimer: This article is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider about your specific medical conditions and treatment options.



a.png)