Total Hip Replacement OVERVIEW
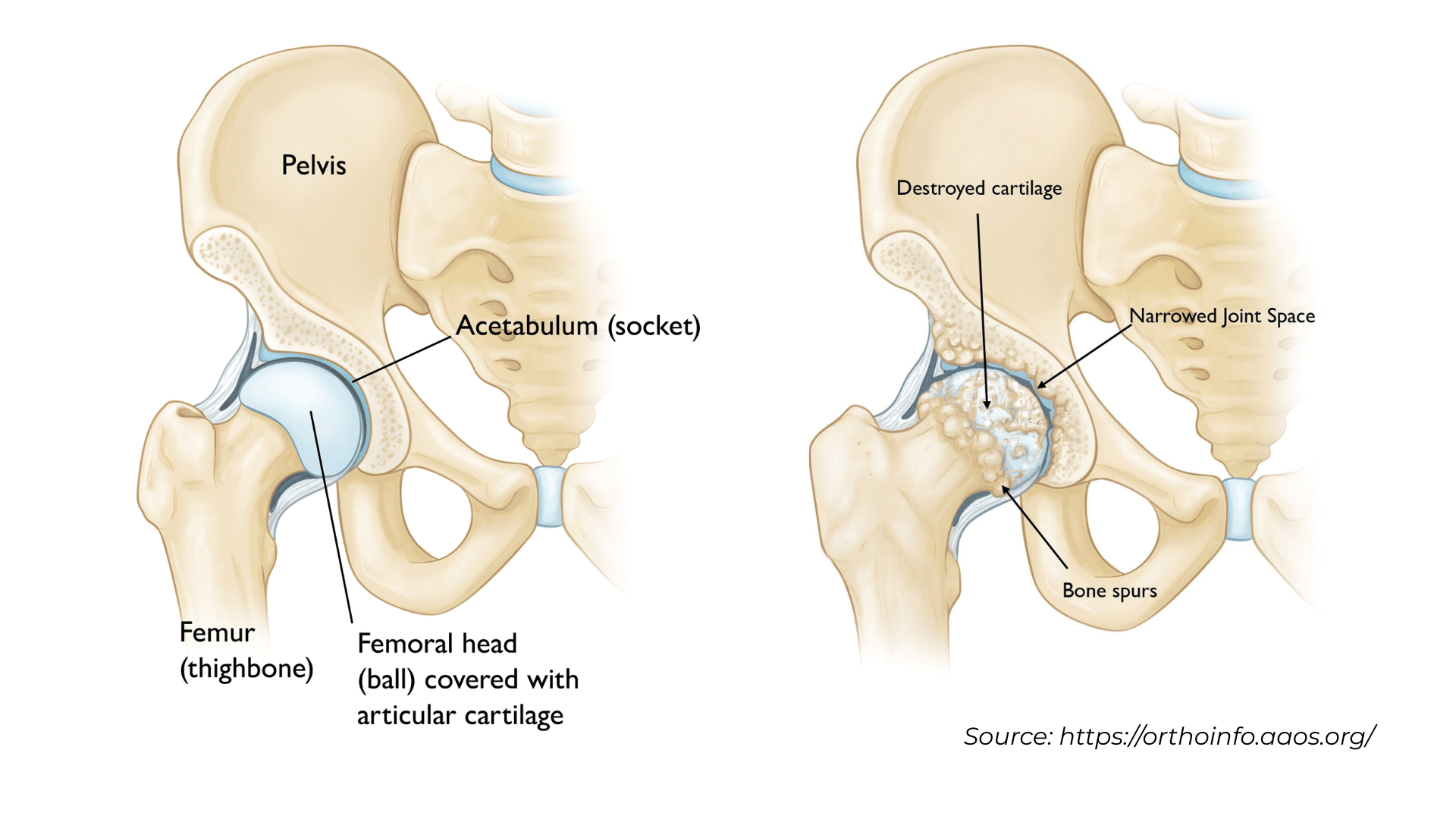
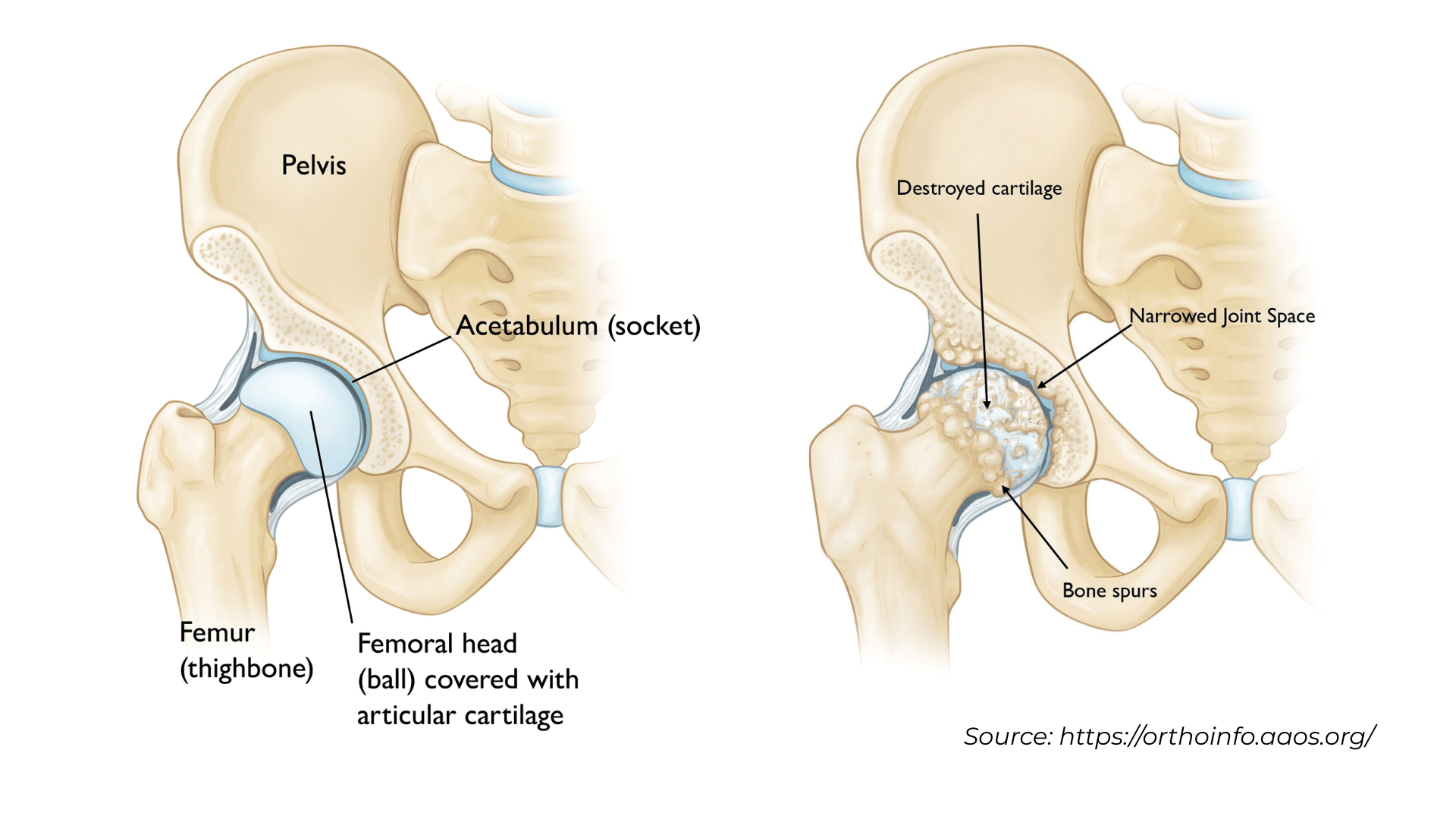
When persistent hip pain and declining joint function interfere with your daily activities in Nashville, Franklin, or throughout Middle Tennessee, despite conservative treatments like medications and physical therapy, it may be time to explore hip replacement surgery options. As a fellowship-trained orthopedic surgeon and Chief of Orthopaedic Surgery at Williamson Medical Center, Dr. Cory Calendine offers patients access to the most advanced total hip replacement techniques available today. Since its introduction in 1960, hip replacement surgery has evolved into one of the most successful procedures in modern medicine, with continued advancements in surgical techniques and robotic technology dramatically improving patient outcomes. During total hip replacement surgery, also called total hip arthroplasty or THA, Dr. Calendine removes damaged bone and cartilage from the hip joint and replaces them with precision-engineered prosthetic components. His expertise in robotic-assisted hip replacement surgery using the Mako system, combined with minimally invasive techniques like the anterior approach, provides patients in the Greater Nashville area with state-of-the-art treatment options designed to optimize recovery and long-term function.
The first step toward hip replacement surgery in Franklin, TN begins with a comprehensive evaluation by Dr. Calendine, a board-certified orthopedic surgeon and founding partner of the Bone and Joint Institute of Tennessee. During your consultation at our Nashville area practice, Dr. Calendine will thoroughly review your medical history, perform a detailed physical examination, and order appropriate imaging studies including X-rays to assess your hip joint condition. Even when patients experience significant hip pain and imaging reveals advanced joint degeneration, conservative treatment approaches are typically explored first as part of comprehensive care. Non-surgical hip treatment options may include appropriate weight management, targeted exercise programs and physical therapy, anti-inflammatory medications, supportive bracing, and therapeutic joint injections. When these conservative measures fail to provide adequate pain relief and functional improvement, total hip replacement surgery becomes a viable consideration. The decision to proceed with hip arthroplasty involves thoughtful consultation between Dr. Calendine, your medical team, and your family to ensure the best treatment approach for your individual situation.
The final decision to undergo total hip replacement surgery is ultimately based on how hip pain and disability impact your quality of life and ability to perform meaningful daily activities. Patients who choose to proceed with hip replacement surgery in Nashville typically report that their symptoms significantly limit essential activities such as walking comfortably, climbing stairs, working productively, sleeping through the night, putting on socks and shoes independently, and sitting for extended periods without discomfort. Dr. Calendine understands that joint replacement surgery represents a major decision, and he works closely with each patient to determine when the benefits of robotic hip replacement surgery outweigh the risks. His expertise in anterior approach hip replacement and Mako robotic technology offers patients in Franklin, Brentwood, and surrounding Tennessee communities access to the most advanced surgical techniques available. When conservative treatments have failed to provide appropriate joint pain relief and hip arthritis continues to interfere with your lifestyle and independence, total hip replacement surgery serves as an effective solution to restore mobility, eliminate pain, and return you to the activities you value most.
description of total hip replacement
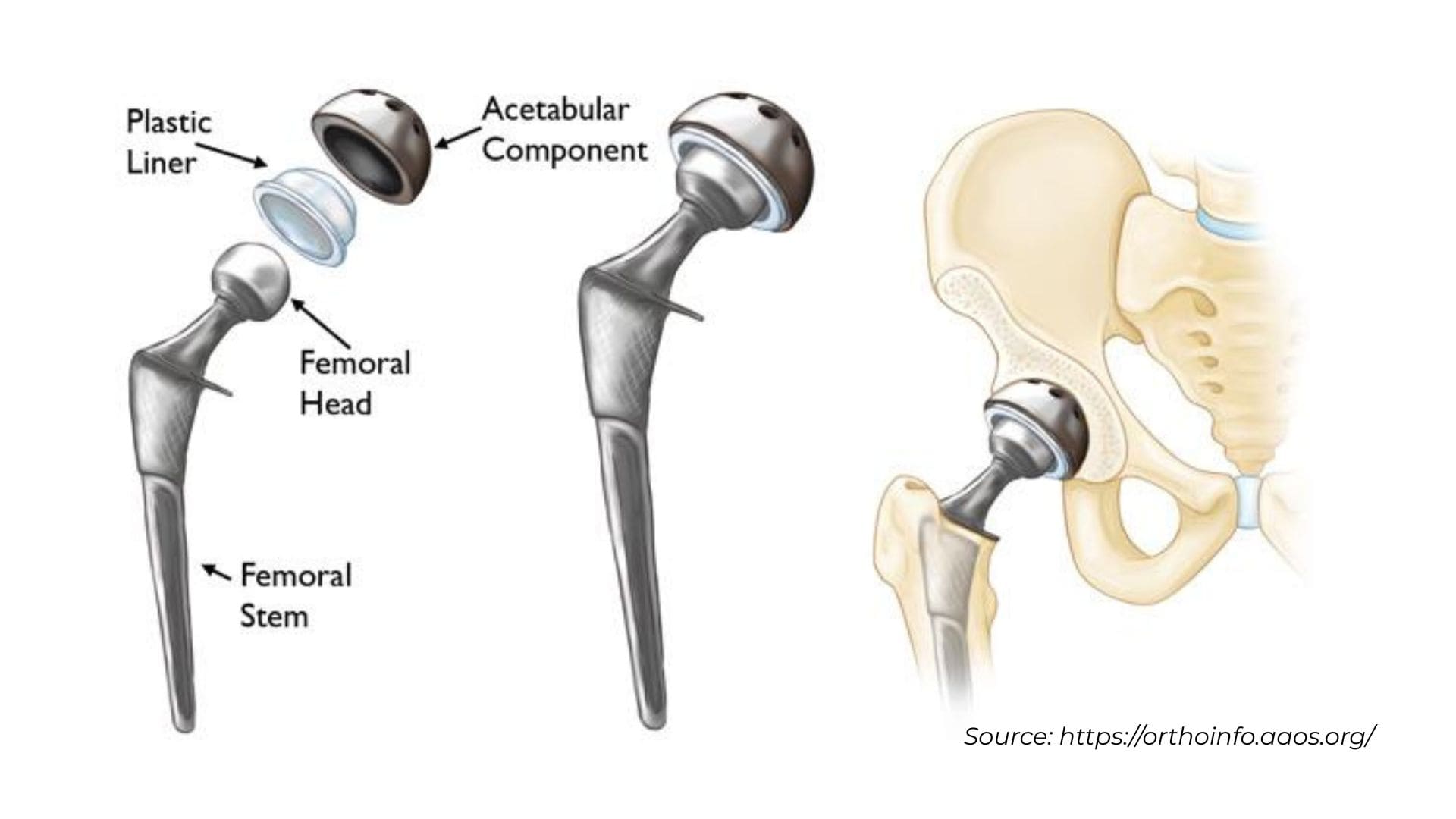
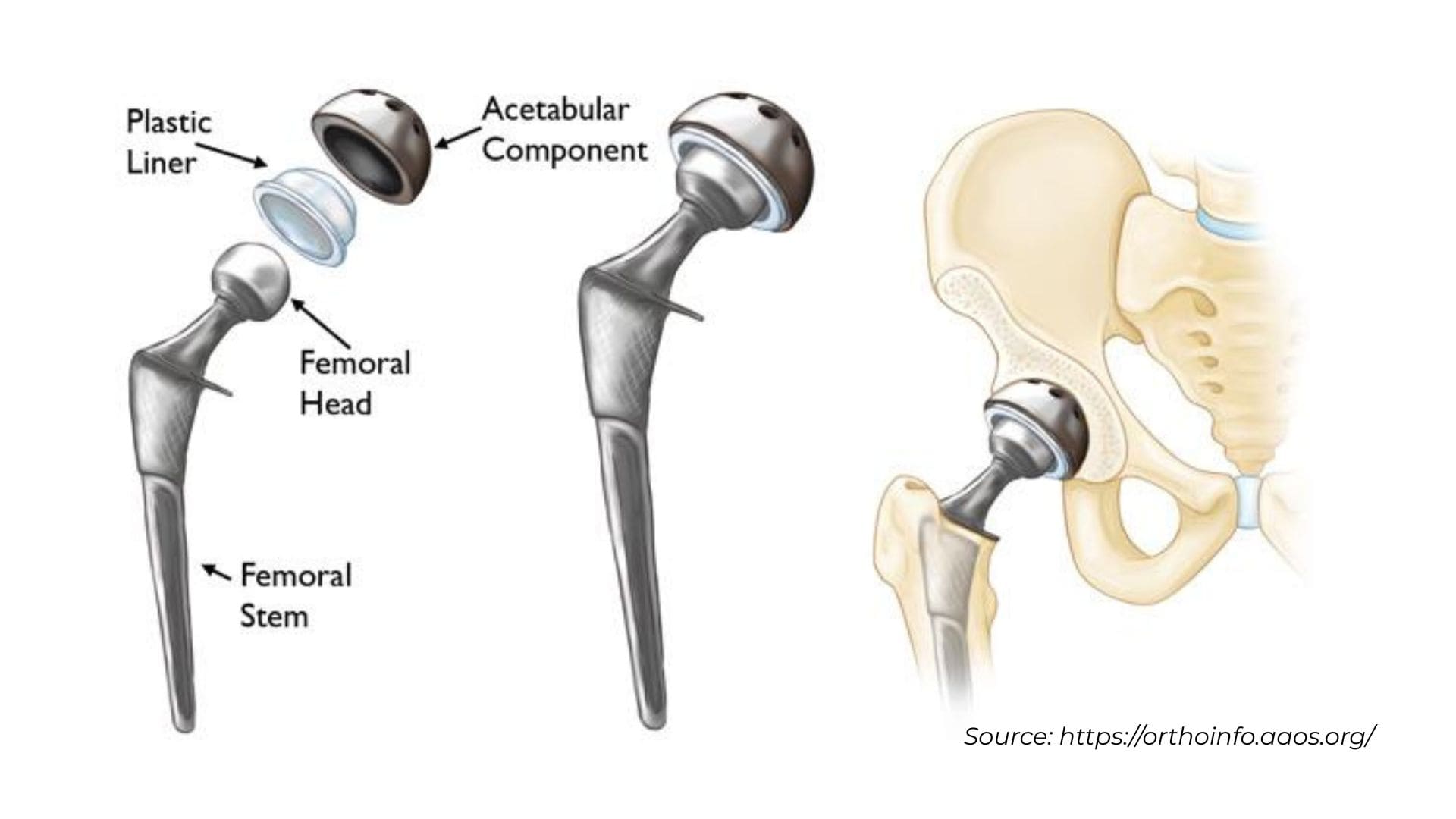
During total hip replacement surgery, also called total hip arthroplasty, Dr. Calendine carefully removes damaged bone and cartilage from your hip joint and replaces them with advanced prosthetic components designed to restore natural movement and eliminate pain. This precise procedure begins with the removal of the damaged femoral head, which Dr. Calendine replaces with a durable metal stem that is securely positioned into the hollow center of the femur or thighbone. Depending on your bone quality and individual anatomy, this femoral stem may be cemented in place or press-fitted into the bone using advanced surgical techniques. At the top of the metal stem, Dr. Calendine attaches a high-quality ceramic ball, or less commonly a metal ball, which serves as the new femoral head to replace the damaged joint surface. The procedure also involves removing the damaged cartilage surface from the hip socket, known as the acetabulum, and replacing it with a precision-engineered metal cup and specialized liner. During robotic-assisted hip replacement surgery in Nashville and Franklin, Tennessee, Dr. Calendine may use screws or cement to secure the metal cup in optimal position for long-term stability. The combination of these plastic, ceramic, and metal components creates a smooth gliding surface that replicates the natural ball-and-socket movement of your original hip joint, allowing patients throughout Middle Tennessee to return to active, pain-free living with improved mobility and function.
Are all hip replacement implants the same?
Modern hip replacement implants (pictured above) used by Dr. Calendine in Nashville and Franklin, Tennessee have evolved through decades of surgical experience and research to determine which designs provide the best long-term outcomes for patients. While most contemporary total hip replacement implants share similar successful design features, an important variable that Dr. Calendine considers for each patient is the bearing surface, which consists of the ball and liner components that attach to the stem and cup fixed to your bone. The ball component of your hip replacement implant can be manufactured from either durable metal, typically a cobalt chromium alloy, or advanced ceramic materials, while the liner can be constructed from medical-grade plastic known as polyethylene, metal, or ceramic. These components can be combined in different configurations for total hip arthroplasty, with combinations named according to their respective materials such as metal-on-polyethylene, ceramic-on-polyethylene, or ceramic-on-ceramic bearings. Currently, the vast majority of hip replacement surgeries performed by Dr. Calendine and orthopedic surgeons nationwide utilize a polyethylene liner paired with either a metal or ceramic ball, as these combinations have demonstrated excellent durability and patient satisfaction. During your consultation for hip replacement surgery in Middle Tennessee, Dr. Calendine will discuss the specific implant options and bearing surface preferences that best match your age, activity level, anatomy, and lifestyle goals to ensure optimal long-term function and durability of your new hip joint.
hip replacement surgical procedure
Below: Dr. Cory Calendine, MD explains the basic components of a Total Hip Replacement.
Hip replacement surgery can typically lasts 1-2 hours. Dr. Calendine will remove the damaged cartilage and bone and then position new metal, plastic, or ceramic implants to restore the alignment and function of your hip. Immediately after surgery, you will be moved to the recovery room where you will remain for a few hours while you recover from anesthesia.
[Read more about anesthesia for hip replacement surgery.] Advances in hip surgery techniques and technology has significantly decreased the amount of time that patients have to spend in the hospital following surgery. Most patients will begin ambulating and moving the joint soon after surgery and some patients will even
go home the same day. This is highly dependent upon your condition before surgery, age, and concurrent medical problems which can influence your recovery and rehabilitation. A safe and personalized discharge plan will be arranged for you by your orthopedic team.
hip replacement recovery
The success of your total hip replacement surgery in Nashville and Franklin, Tennessee depends significantly on your physical condition before surgery and your commitment to following Dr. Calendine's comprehensive post-operative care instructions during the critical first weeks of recovery. As Chief of Orthopaedic Surgery at Williamson Medical Center, Dr. Calendine and his experienced medical team prioritize early mobilization and getting patients out of bed as quickly as safely possible following robotic hip replacement surgery. Most hip replacement patients at our Middle Tennessee surgical center are walking with the assistance of a walker on the day of surgery or the following day, a practice that has proven essential for accelerating post-operative recovery and significantly reducing the risk of complications such as blood clots. The progression from using a walker to a cane, or walking independently without assistance, typically occurs within the first 4-6 weeks after anterior approach hip replacement surgery, though individual recovery timelines may vary based on each patient's healing progress, commitment to physical therapy, and overall health status. Surgical wound care represents another crucial aspect of successful hip replacement recovery, with stitches or staples typically removed within 2 weeks following your procedure at our Franklin, TN practice. Dr. Calendine's team provides detailed home wound care instructions that are carefully explained prior to your discharge and included in your personalized written care plan, ensuring you have the knowledge and confidence needed for optimal healing and the best possible outcome from your total hip replacement surgery.
[Read more about what to expect the first week following hip replacement surgery.]The majority of Total Hip Replacement surgery patients are able to participate in most of their daily activities within six weeks. Dr. Calendine typically allows patients to drive at four to six weeks after surgery and sometimes sooner (especially if the operative leg is the left leg). There is some literature that states that your reaction time will not be back to normal prior to six weeks. You should not drive while on narcotics, and should discuss returning to driving with your operating surgeon. By three months, most people have regained much of the endurance and strength lost around the time of surgery, and can participate in daily activities with few restriction. Even after daily activities have resumed, it is important to avoid high impact activities to give you the best long-term outcome with your hip. Returning to work is highly dependent on your general health, activity level and demands of your job. If you have a sedentary job, such as computer work, you can expect to return to work in four to six weeks. If you have a more demanding job that requires lifting, walking, or travel, you may need up to three months for full recovery.
physical therapy following Total hip replacement
Following your total hip replacement surgery in Nashville or Franklin, Tennessee, you will receive immediate physical therapy assistance while recovering at Williamson Medical Center to help you safely begin walking and regain mobility. Depending on your pre-operative physical conditioning, support system at home, and individual healing progress, Dr. Calendine may recommend additional outpatient physical therapy to optimize your recovery from hip replacement surgery. Much of the rehabilitation after total hip arthroplasty focuses on progressive walking programs, gentle stretching exercises, and targeted thigh muscle strengthening activities that many patients can successfully perform independently at home without requiring ongoing physical therapist supervision. Dr. Calendine's expertise in
anterior approach hip replacement surgery provides significant advantages for patients throughout Middle Tennessee, as this advanced minimally invasive technique dramatically decreases your risk of implant dislocation and reduces activity restrictions immediately following surgery. Post-operative precautions and activity guidelines will be personalized for each patient based on the specific surgical approach performed, your individual anatomy, healing progress, and any concurrent medical conditions that may influence your recovery timeline. Prior to your discharge from our Nashville area hospital, Dr. Calendine and your dedicated medical care team will provide you with detailed, written instructions outlining any specific precautions you need to follow, ensuring you have clear guidance for a safe and successful recovery from your anterior approach hip replacement surgery in Franklin, TN.
follow-up and precautions following hip replacement
Fall prevention remains a top priority during the first few weeks following your total hip replacement surgery in Nashville and Franklin, Tennessee, as your new hip joint continues to heal and strengthen. Stairs present a particular challenge during early hip replacement recovery until your new hip develops adequate strength and mobility for safe navigation. Patients recovering from anterior approach hip replacement surgery should consistently use appropriate assistive devices such as a cane, crutches, walker, or handrails, and have someone available to provide assistance until balance, flexibility, and hip strength show significant improvement. Dr. Calendine and the experienced physical therapy team at the Bone and Joint Institute of Tennessee will provide expert guidance on selecting the most appropriate assistance device for your individual needs and ensure you understand proper techniques for safe use throughout your recovery period. This personalized approach to hip replacement rehabilitation helps minimize fall risk while optimizing your return to normal activities in Middle Tennessee.
Follow-up care after your total hip replacement surgery is vitally important to ensure optimal recovery and long-term success of your new hip joint. As Chief of Orthopaedic Surgery at Williamson Medical Center, Dr. Calendine understands that the frequency and timing of follow-up visits after hip replacement surgery depends on numerous individual factors including your age, any complications that may arise, the activity demands you place on your new joint, and the specific type of robotic hip replacement procedure completed. Dr. Calendine and your dedicated medical team at our Franklin, TN practice will carefully evaluate each of these factors and develop a personalized follow-up schedule tailored to best serve your unique recovery needs and ensure the continued success of your total hip arthroplasty. This individualized approach to post-operative care reflects Dr. Calendine's commitment to providing comprehensive, patient-centered orthopedic care throughout the Greater Nashville area.
Additional total hip replacement resources:
Source:
American Academy of Orthopaedic Surgeons, https://orthoinfo.aaos.org/; American Association of Hip and Knee Surgeons, https://hipknee.aahks.org/total-hip-replacement/