Understanding Femoral Neck Fractures: Types, Treatment, and Recovery Options
Summary: Femoral neck fractures are serious injuries to the upper portion of the thigh bone where it connects to the hip joint, commonly affecting older adults due to falls and bone weakness. These fractures disrupt the blood supply to the femoral head and carry significant risks of complications like avascular necrosis and nonunion. Treatment depends on the patient's age, fracture type, and activity level, ranging from surgical repair with screws in younger patients to hip replacement in older adults, with prompt medical attention being critical for optimal outcomes.
What You Need to Know About Femoral Neck Fractures
When I see patients in my office with hip pain after a fall, one of my biggest concerns is a femoral neck fracture. These injuries affect the narrow section of your thigh bone (femur) that connects the rounded ball of your hip joint to the main shaft of the bone. Think of it as the "neck" that holds your hip's ball-and-socket joint together.
Here's what makes these fractures particularly challenging: the femoral neck sits inside your hip joint capsule, bathed in joint fluid rather than surrounded by the rich blood supply that helps most bones heal. This location creates unique healing challenges that we need to address quickly and effectively.
In my years of treating orthopedic patients, I've learned that understanding your specific type of femoral neck fracture helps you make informed decisions about treatment and recovery. Let me walk you through what you need to know.
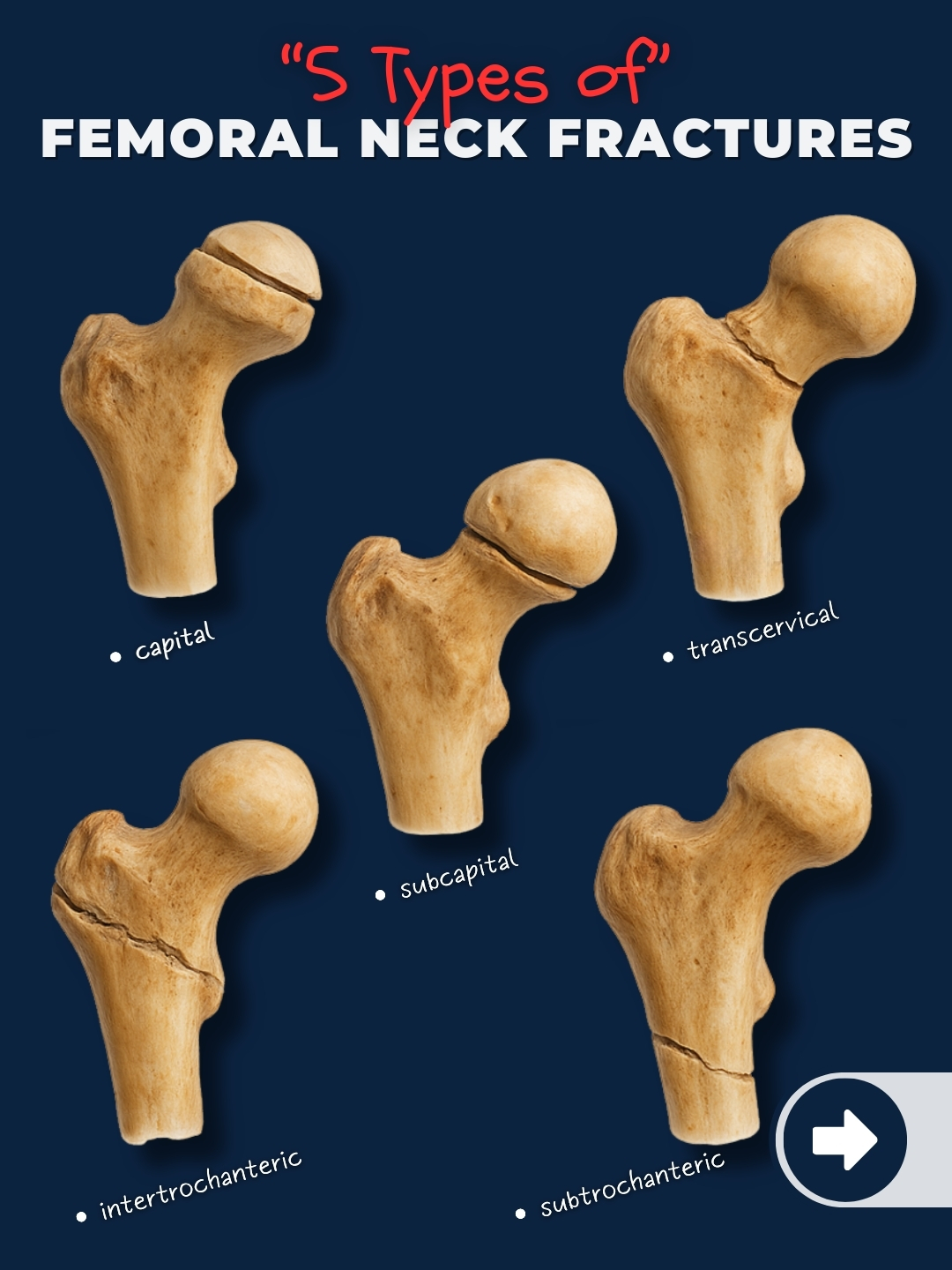
The Different Types of Femoral Neck Fractures
Location-Based Classification
Your femoral neck fracture falls into one of three main categories based on where the break occurs:
Subcapital Fractures happen right at the junction where the femoral head meets the neck. These fractures sit closest to the hip joint and have the highest risk of disrupting blood flow to the femoral head. When I diagnose a subcapital fracture, I'm particularly concerned about the potential for avascular necrosis, where part of the bone dies due to lack of blood supply.
Transcervical Fractures occur through the middle portion of the femoral neck. These represent the most common type I see in my practice. The fracture line runs directly across the narrowest part of the neck, creating stability challenges that often require surgical intervention.
Basicervical Fractures happen at the base of the femoral neck, closer to the main shaft of your thigh bone. While these fractures have better blood supply than the other types, they can be mechanically unstable and may require different treatment approaches.
Garden Classification System
As an orthopedic surgeon, I use the Garden classification to communicate with other doctors about your fracture's severity. This system grades fractures from I to IV based on displacement:
Garden I fractures are incomplete, valgus-impacted fractures. You might have significant pain, but the bone fragments remain in good position. These often have the best prognosis for healing without surgery in select patients.
Garden II fractures are complete but nondisplaced. The bone is broken all the way through, but the pieces haven't shifted out of place. These fractures walk a fine line—they may heal well with surgery, but there's risk of displacement if left untreated.
Garden III fractures show partial displacement. The bone fragments have shifted somewhat, compromising the blood supply and requiring more aggressive treatment to prevent complications.
Garden IV fractures are completely displaced. The bone ends have separated significantly, almost certainly disrupting the blood vessels that feed the femoral head. These represent the most serious type and typically require joint replacement rather than repair.
How These Fractures Happen and Who's at Risk
Common Causes by Age Group
In my practice, I see two distinct patterns. Older patients typically sustain femoral neck fractures from relatively minor falls—sometimes just stepping off a curb wrong or tripping over a rug. The underlying bone weakness from osteoporosis makes even low-energy impacts dangerous.
Younger patients usually require significant trauma like motor vehicle accidents or falls from height. When I treat a femoral neck fracture in someone under 50, I'm immediately thinking about preserving their hip joint for the long term, as they'll need it to last many decades.
Risk Factors You Should Know
Several factors increase your risk of femoral neck fractures. Age is the biggest factor—your risk increases exponentially after age 65. Women face higher risk than men, particularly after menopause when estrogen levels drop and bone density decreases.
Medical conditions like osteoporosis, rheumatoid arthritis, and certain medications (especially long-term steroids) weaken your bones. If you've had previous fractures, especially hip fractures, your risk is elevated. Lifestyle factors like smoking, excessive alcohol consumption, and lack of physical activity also contribute to fracture risk.
Treatment Options: Finding the Right Approach for You
Non-Surgical Treatment: When Rest Makes Sense
Occasionally, I recommend non-surgical treatment for very specific situations. This might be appropriate if you're non-ambulatory and have significant medical conditions that make surgery extremely risky. However, I want to be clear—non-surgical treatment for displaced femoral neck fractures usually leads to poor outcomes.
For nondisplaced fractures in very select patients, we might try protected weight-bearing with close monitoring. But even then, many of these fractures will eventually require surgery.
Surgical Repair: Saving Your Natural Hip Joint
When I can preserve your natural hip joint, that's usually my first choice, especially for younger patients or those with nondisplaced fractures.
Cannulated Screw Fixation works well for stable, nondisplaced fractures. I place three precisely positioned screws across the fracture to hold the bone fragments together while healing occurs. The surgery is relatively quick, and you can often bear weight soon after surgery.
Sliding Hip Screws provide excellent stability for certain fracture patterns, particularly basicervical fractures. This implant includes a large screw that slides within a barrel, allowing controlled compression at the fracture site as you heal.
Joint Replacement: When a New Hip is Best
For many displaced fractures, especially in older patients, hip replacement offers the most predictable results.
Hemiarthroplasty replaces just the femoral head and neck, leaving your natural hip socket in place. This works well for less active patients and has a lower dislocation risk than total hip replacement.
Total Hip Arthroplasty replaces both the ball and socket of your hip joint. I typically recommend this for more active patients or those with pre-existing hip arthritis. While it has a slightly higher dislocation risk, it provides excellent pain relief and function.
When to Seek Immediate Medical Care
If you're experiencing severe hip or groin pain after a fall, especially if you can't bear weight on that leg, you need immediate medical evaluation. Don't wait to see if the pain improves—time matters significantly with femoral neck fractures.
Watch for these warning signs: inability to lift your leg, visible shortening or external rotation of your leg, severe pain with any hip movement, or inability to walk. In elderly patients, sometimes the only symptom is refusing to walk or increased confusion.
Even if your X-rays initially appear normal but you have persistent hip pain and difficulty walking, insist on further evaluation. Some femoral neck fractures don't show up clearly on initial X-rays, and MRI or CT scans may be necessary.
Recovery and Lifestyle Considerations
What to Expect During Healing
Recovery timelines vary significantly based on your fracture type and treatment. If you have internal fixation surgery, bone healing typically takes 3-6 months. During this time, you'll likely need physical therapy to regain strength and mobility.
Hip replacement patients often see faster initial improvement in pain and function, but complete recovery still takes several months. I tell my patients that while you might feel great at 6 weeks, your body continues healing and strengthening for up to a year.
Preventing Future Fractures
After treating your femoral neck fracture, preventing future injuries becomes a priority. If you have osteoporosis, work with your primary care doctor to address bone density through medications, calcium, and vitamin D supplementation.
Exercise plays a crucial role in both bone health and fall prevention. Weight-bearing activities like walking help maintain bone density, while balance training reduces fall risk. I often refer patients to physical therapy specifically for balance and fall prevention programs.
Home safety modifications can prevent many falls. Remove throw rugs, improve lighting, install grab bars in bathrooms, and consider a medical alert system if you live alone.
Long-term Outlook
With appropriate treatment, most patients can return to their previous activity levels, though this may take time. Younger patients with successfully healed fractures often regain full function. Older patients may experience some permanent changes in mobility, but most can return to independent living.
The key is realistic expectations and patience with the healing process. Your bones, muscles, and overall conditioning need time to recover fully. Don't rush the process—gradual, steady progress leads to the best long-term outcomes.
Taking Control of Your Recovery
Femoral neck fractures represent serious injuries that require prompt, expert treatment. Understanding your specific fracture type helps you make informed decisions about treatment options and set appropriate expectations for recovery.
The most important message I share with patients is this: early intervention and appropriate treatment dramatically improve your chances of a successful outcome. Whether you need fracture repair or joint replacement, modern orthopedic techniques offer excellent results when applied correctly.
If you're dealing with a femoral neck fracture, don't hesitate to ask questions about your treatment options. Understanding your injury and treatment plan helps you participate actively in your recovery and achieve the best possible outcome.
Remember, while femoral neck fractures are serious, they're also very treatable with today's surgical techniques and rehabilitation programs. With proper care and dedication to your recovery plan, you can look forward to returning to the activities you enjoy.
Dr. Cory Calendine specializes in orthopedic surgery and has extensive experience treating hip fractures and joint replacement. If you're experiencing hip pain or have concerns about fracture risk, contact our office to schedule a consultation and discuss your treatment options.








