partial knee Replacement OVERVIEW
When knee arthritis affects only one area of your joint, Dr. Cory Calendine offers Nashville and Franklin patients an innovative alternative to total knee replacement that can get you back to your active Middle Tennessee lifestyle faster. As one of the region's leading Mako robotic surgery specialists at Williamson Medical Center, Dr. Calendine performs partial knee replacement surgery with precision that preserves more of your natural knee while delivering exceptional pain relief and improved function.
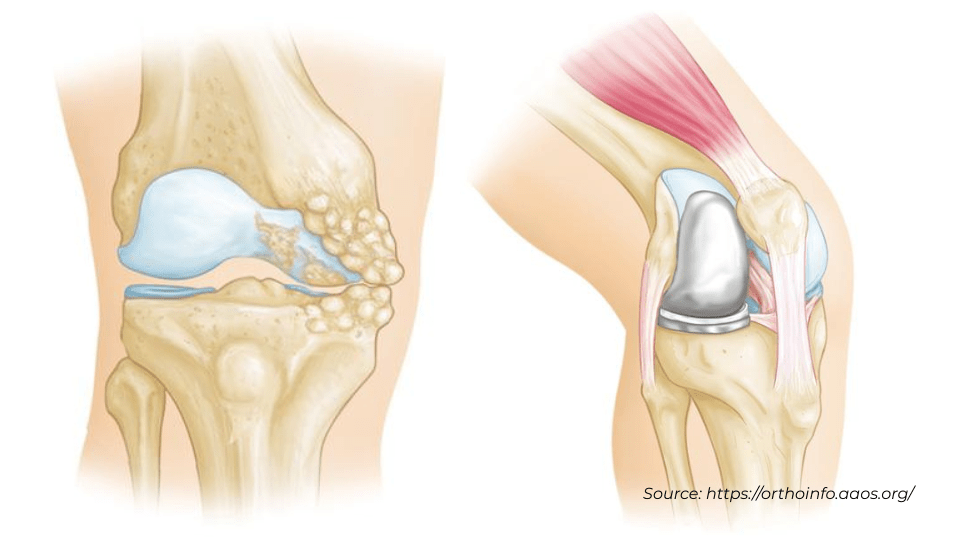
Dr. Calendine has helped hundreds of Greater Nashville area patients understand the important differences between partial and total knee replacement surgery. Your knee joint consists of three distinct compartments: the inner side (medial), outer side (lateral), and the area under your kneecap (patellofemoral). When arthritis affects only one of these compartments, partial knee replacement allows Dr. Calendine to replace just the damaged area while preserving your healthy knee tissue and natural ligaments.
This targeted approach means that partial knee replacement is essentially one-third of the surgery required for total knee replacement, offering Nashville patients several compelling advantages. Using advanced Mako robotic technology, Dr. Calendine can perform partial knee replacement through a smaller incision, resulting in less surgical trauma, reduced pain, and faster recovery times compared to traditional total knee replacement.
Patients throughout Franklin and Middle Tennessee choose Dr. Calendine for partial knee replacement because of his expertise with the advanced Mako robotic system. This cutting-edge technology allows for unprecedented precision in preserving your healthy bone and soft tissue while ensuring optimal placement of your new partial knee implant. Most of Dr. Calendine's partial knee replacement patients experience shorter hospital stays, quicker return to daily activities, and higher satisfaction rates compared to total knee replacement patients.
The robotic-assisted approach also reduces surgical complications such as blood loss and the risk of blood clots, while the smaller incision results in less scarring and faster healing. Many Nashville-area patients are amazed at how quickly they can return to activities like walking, climbing stairs, and even recreational sports after their Mako partial knee replacement with Dr. Calendine.
Making the Right Choice for Your Nashville Lifestyle
Dr. Calendine believes in providing his patients with complete information to make the best decision for their individual situation. While partial knee replacement offers faster recovery and preservation of your natural knee, it's important to understand that the lifespan of partial knee components may be shorter than total knee replacements. However, if revision surgery is ever needed, Dr. Calendine can successfully convert a partial knee replacement to a total knee replacement with excellent outcomes.
As a fellowship-trained orthopedic surgeon serving the Bone and Joint Institute of Tennessee, Dr. Calendine will thoroughly evaluate your specific arthritis pattern, activity level, and goals to determine whether partial knee replacement is the right choice for your active Middle Tennessee lifestyle.
description of partial knee replacement
Dr. Calendine often explains to his patients that partial knee replacement surgery is more accurately described as knee "resurfacing," since only the damaged surfaces of your bones are replaced while preserving the healthy portions of your knee joint. This precision-focused approach, enhanced by Mako robotic technology at Williamson Medical Center, allows Dr. Calendine to restore your knee function while maintaining as much of your natural anatomy as possible.
The partial knee replacement process begins with Dr. Calendine carefully preparing the bone surfaces using the advanced Mako robotic system. The damaged cartilage at the ends of your thigh bone (femur) and shin bone (tibia) is precisely removed along with a minimal amount of underlying bone, guided by the robotic arm's real-time feedback. This computer-assisted precision ensures that Dr. Calendine removes only the damaged tissue while preserving maximum healthy bone and cartilage throughout your knee joint.
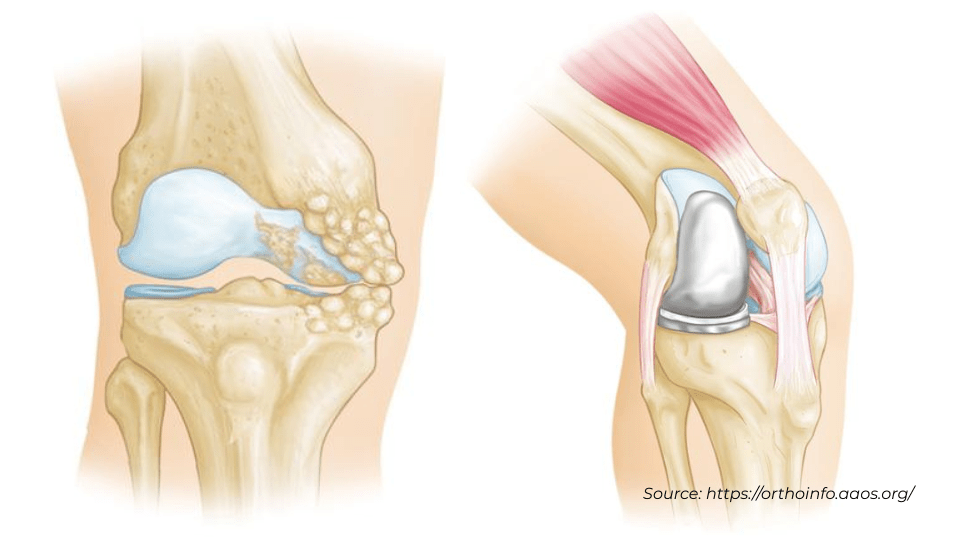
Once the bone preparation is complete, Dr. Calendine positions the metal implant components with exceptional accuracy using Mako robotic guidance. These specially designed metal parts recreate the smooth surface of your natural joint, and depending on your specific case and bone quality, they may be secured using bone cement or through a "press-fit" technique that allows your bone to grow into the implant over time. The robotic system's precision helps ensure optimal implant alignment, which is crucial for long-term success and natural knee movement.
Depending on the extent of your arthritis and the condition of your kneecap, Dr. Calendine may also resurface the undersurface of your patella (kneecap) during your partial knee replacement surgery. When this step is necessary, he carefully cuts and resurfaces this area with a smooth plastic component that works seamlessly with your new partial knee implant. Dr. Calendine makes this decision based on your individual anatomy and arthritis pattern, always focusing on what will provide you with the best long-term outcomes.
The final step involves Dr. Calendine inserting a medical-grade plastic spacer between the metal components, creating a smooth gliding surface that mimics the function of your natural knee cartilage. This ultra-high molecular weight polyethylene spacer is designed to provide years of smooth, pain-free movement, allowing you to return to your active Middle Tennessee lifestyle with confidence. The precision of the Mako robotic system ensures that all components work together harmoniously, providing you with optimal knee function and longevity.
Proven Results with Mako Partial Knee Replacement in Nashville
Extensive clinical research consistently demonstrates that carefully selected patients achieve excellent results with partial knee replacement surgery, and Dr. Calendine's experience with hundreds of Nashville and Franklin patients confirms these positive outcomes. The advanced Mako robotic technology that Dr. Calendine uses at Williamson Medical Center has further enhanced these results, providing even greater precision in patient selection and surgical execution for optimal long-term success.
The advantages of Dr. Calendine's Mako robotic partial knee replacement approach over traditional total knee replacement are significant for appropriately selected Middle Tennessee patients. Recovery times are notably quicker, with most patients experiencing less post-operative pain and reduced blood loss compared to total knee replacement surgery. Perhaps most importantly, because Dr. Calendine's partial knee replacement technique preserves your healthy bone, cartilage, and ligaments, the vast majority of his Greater Nashville area patients report that their new knee feels remarkably natural and often achieves better range of motion than what's typically possible with total knee replacement.
Making an Informed Decision About Your Knee Replacement Options
Dr. Calendine believes in providing his patients with complete transparency about all treatment options. While partial knee replacement offers many advantages, he ensures that patients understand that pain relief can be slightly less predictable compared to total knee replacement, and there's a possibility that arthritis may develop in the untreated portions of the knee over time, potentially requiring conversion to total knee replacement in the future. However, Dr. Calendine's extensive experience has shown that when this occurs, the conversion surgery is highly successful and patients achieve excellent outcomes.
Both partial and total knee replacement procedures can provide outstanding results when performed by an experienced surgeon like Dr. Calendine using advanced Mako robotic technology. The key to success lies in careful patient selection, precise surgical technique, and setting appropriate expectations. Dr. Calendine takes time during consultations at the Bone and Joint Institute of Tennessee to thoroughly discuss the risks and benefits of each surgical option, ensuring that your choice aligns with your lifestyle, activity goals, and long-term expectations for your Middle Tennessee lifestyle.
Regardless of which knee replacement option you and Dr. Calendine decide is best for your situation, following post-operative guidelines and activity restrictions is essential for maximizing the longevity of your new knee. While these procedures are designed to restore function and eliminate pain for daily activities and low-impact recreational pursuits, neither partial nor total knee replacement is intended for high-impact sports. With proper care and adherence to Dr. Calendine's post-operative instructions, your knee replacement can provide decades of pain-free function, allowing you to maintain an active, fulfilling lifestyle throughout the Nashville area.
partial knee replacement surgical procedure
Source:
American Academy of Orthopaedic Surgeons, https://orthoinfo.aaos.org/; American Association of Hip and Knee Surgeons, https://hipknee.aahks.org/total-hip-replacement/Cory Calendine, MD is an Orthopedic Surgeon and founding partner of the Bone and Joint Institute of Tennessee at Williamson County Hospital in Franklin, TN. Dr. Calendine is an expert in Joint Replacement, specializing in Hip and Knee Surgery. From diagnosis through treatment, the Orthopedic Surgical experts at the Bone and Joint Institute use the latest techniques and technology to improve care for people with musculoskeletal problems. For more information, please contact our office or schedule your appointment today.