partial Hip Replacement for fracture OVERVIEW
Partial hip replacement, also known as hip hemiarthroplasty, is a specialized surgical procedure performed by Dr. Calendine in Nashville and Franklin, Tennessee, where only the femoral head, or ball portion of the damaged hip joint, is replaced with a prosthetic component. Unlike total hip replacement surgery, partial hip replacement preserves the patient's natural acetabulum, which is the socket portion of the hip joint. Dr. Calendine, serving as Chief of Orthopaedic Surgery at Williamson Medical Center, primarily performs hip hemiarthroplasty to treat femoral neck fractures, which are a specific type of hip fracture commonly seen in elderly patients or those who have experienced traumatic injury. During partial hip replacement surgery in Middle Tennessee, only the head of the femur or thigh bone is replaced with an artificial component, and the new prosthetic femoral head is designed to rotate smoothly within the body's own natural hip socket, preserving healthy bone and cartilage when possible.
The hip implant used in partial hip replacement surgery consists of a high-quality ceramic or metal ball that is securely attached to a precisely engineered metal stem. Dr. Calendine carefully positions this metal stem down into the core of the thighbone, or femur, ensuring optimal stability and function for patients throughout the Greater Nashville area. This partial hip replacement technique allows the prosthetic femoral head to move naturally within the patient's original hip socket, maintaining normal hip mechanics while replacing only the damaged portion of the joint. The surgical approach for hip hemiarthroplasty requires specialized expertise to ensure proper implant positioning and alignment, which Dr. Calendine has developed through extensive training and experience in hip fracture surgery and joint replacement procedures.
partial versus total hip replacement
The key distinction between partial hip replacement and total hip replacement lies in the extent of joint reconstruction required for each patient's specific condition. While partial hip replacement surgery in Franklin, TN involves replacing only the femoral head and preserving the natural socket, total hip replacement requires replacing both the femoral head and resurfacing the acetabular socket with prosthetic components. In total hip replacement procedures, the prosthetic femoral head moves within a prosthetic socket, creating an entirely artificial joint system. Dr. Calendine most commonly performs total hip replacement surgery when there is significant cartilage damage affecting both the femoral head and the socket, which typically occurs from degenerative osteoarthritis of the hip joint. However, there is an increasing trend in orthopedic surgery to treat certain types of hip fractures with total hip replacement rather than partial hip replacement, particularly in younger, more active patients who may benefit from the enhanced longevity and function of a complete joint replacement. During your consultation for hip surgery in the Nashville area, Dr. Calendine will carefully evaluate your specific condition, age, activity level, and overall health to determine whether partial hip replacement or total hip replacement provides the best long-term outcome for your individual situation.
types of hip fractures
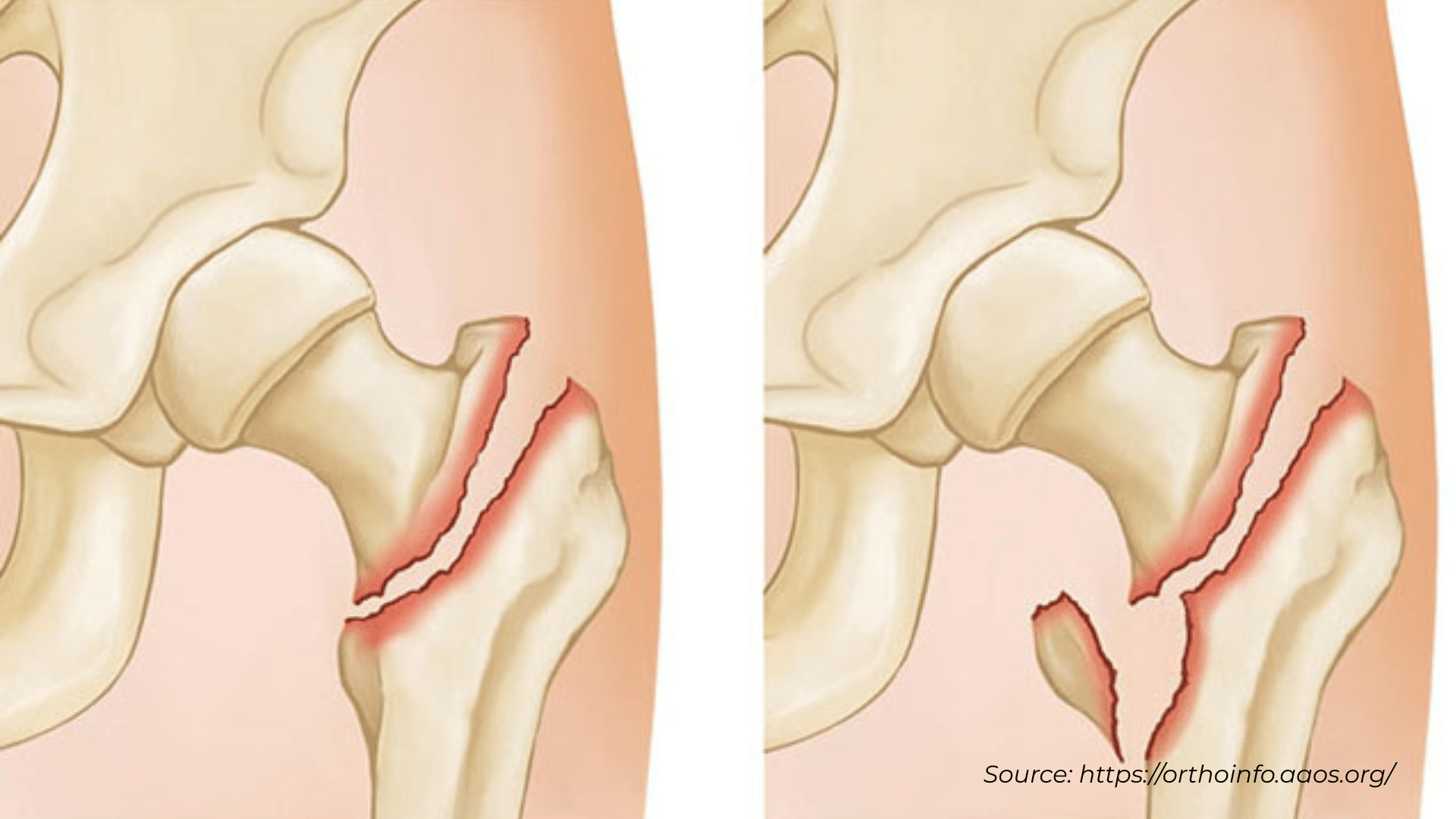
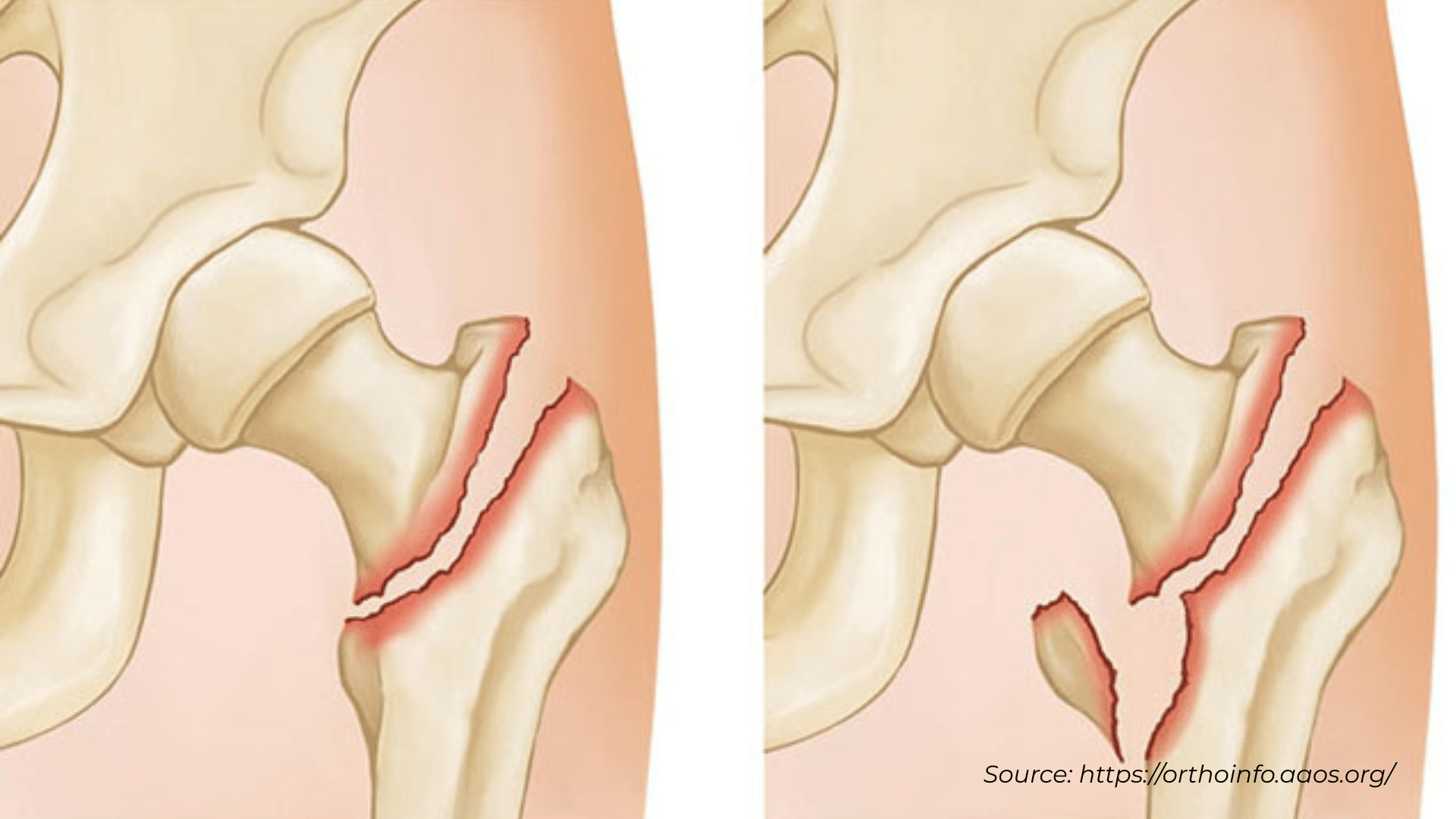
Dr. Calendine, serving patients with hip fractures in Nashville and Franklin, Tennessee, explains that hip fractures are classified into four distinct categories or grades based on their location and severity. Grades 1, 2, and 3 hip fractures include subtrochanteric, intertrochanteric, and fractured neck injuries that do not interfere with the hip joint itself and can generally be successfully repaired using surgical pins or specialized nailing devices at Williamson Medical Center. Grade 4 hip fractures, known as subcapital fractures, present more complex challenges and are further classified into four types based on the amount of bone displacement that occurs at the fracture site. Dr. Calendine's expertise in hip fracture surgery throughout Middle Tennessee enables him to determine the most appropriate treatment approach for each specific fracture pattern and patient condition.
The four types of subcapital hip fractures treated by Dr. Calendine require different surgical approaches based on bone displacement and stability. Type 1 subcapital fractures are stable fractures with impaction, meaning the bone fragments are pressed together and maintain good contact, allowing for successful repair with surgical pins or screws. Type 2 fractures are complete but non-displaced, meaning the bones remain properly aligned as they were before the fracture occurred, making them suitable candidates for internal fixation procedures. Type 3 subcapital fractures are displaced but the two bone fragments maintain some contact with one another, often allowing for successful surgical repair using pins or nailing devices. However, Type 4 subcapital fractures are completely displaced with no contact between the fracture fragments, creating a situation where the blood supply to the femoral head is disrupted, leading to early bone death or avascular necrosis. This type of severe hip fracture in Franklin, TN is highly unlikely to heal properly if treated with pins like the other fracture categories, making partial hip replacement or hemiarthroplasty the preferred treatment option.
When Dr. Calendine determines that a Type 4 subcapital hip fracture has disrupted the blood supply to the femoral head, partial hip replacement surgery becomes the most effective treatment option for patients in the Greater Nashville area. Hip hemiarthroplasty performed by Dr. Calendine involves carefully removing the broken femoral head, trimming the fractured end of the femoral neck, and inserting a single-piece prosthesis consisting of a metal stem and ceramic or metal ball component. This partial hip replacement technique preserves the patient's natural hip socket or acetabulum, which typically remains in excellent condition despite the fracture, allowing for optimal function and recovery. The advantage of hemiarthroplasty for severe hip fractures is that it provides immediate stability and pain relief while preserving healthy bone and cartilage, enabling patients to return to weight-bearing activities much sooner than would be possible with other treatment approaches. Dr. Calendine's experience in both hip fracture repair and partial hip replacement surgery ensures that patients receive the most appropriate treatment based on their specific fracture pattern, age, activity level, and overall health status.
symptoms of hip fracture
Patients with hip fractures seeking treatment from Dr. Calendine in Nashville and Franklin, Tennessee typically experience characteristic pain patterns over the outer upper thigh or in the groin area that worsen with movement. Hip fracture patients throughout Middle Tennessee report significant discomfort and inability to bear weight when attempting to flex or rotate the injured hip joint. Dr. Calendine, Chief of Orthopaedic Surgery at Williamson Medical Center, explains that when the hip bone has been weakened by underlying disease such as osteoporosis, stress injuries, or cancer, patients may notice persistent aching in the groin or thigh area for a period of time before the actual fracture occurs. In cases where the hip bone is completely fractured, the injured leg may appear noticeably shorter than the non-injured leg due to muscle spasm and bone displacement. Patients with hip fractures often instinctively hold the injured leg in a still, protective position with the foot and knee turned outward in external rotation to minimize pain and prevent further injury. If you experience these hip fracture symptoms in the Greater Nashville area, immediate medical evaluation by an experienced orthopedic surgeon like Dr. Calendine is essential for proper diagnosis and treatment to prevent complications and ensure optimal recovery.
partial vs. total hip replacement for fracture
While partial hip replacement or hemiarthroplasty can be an effective treatment for certain hip fractures, Dr. Calendine explains that younger patients who suffer Type 4 subcapital fractures in Nashville and Franklin, Tennessee may be better candidates for total hip replacement surgery instead. The concern with partial hip replacement in younger, active patients is that the metal prosthetic head bearing against natural bone can result in accelerated wear on the acetabular socket over time, potentially wearing away the base of the socket and requiring additional surgery. For this reason, Dr. Calendine, serving as Chief of Orthopaedic Surgery at Williamson Medical Center, may recommend total hip replacement as an emergency procedure rather than partial hip replacement for younger patients and very active older patients who are likely to place higher demands on their hip joint. This approach helps ensure optimal long-term function and reduces the likelihood of future complications or the need for revision surgery in active individuals throughout Middle Tennessee.
Dr. Calendine typically recommends partial hip replacement surgery for carefully selected patients who meet specific criteria that make them excellent candidates for this procedure. Ideal candidates for hip hemiarthroplasty in the Greater Nashville area generally have no underlying hip arthritis and possess healthy acetabular cartilage that can function well with the prosthetic femoral head. This situation is commonly seen in elderly patients who have fractured the femoral neck after a fall but did not experience troublesome hip symptoms or hip arthritis prior to their injury. Partial hip replacement is particularly well-suited for patients who have sustained an isolated femoral neck fracture without pre-existing joint disease, allowing them to maintain their natural hip socket while replacing only the damaged femoral head component.
Dr. Calendine carefully evaluates multiple factors when determining whether partial hip replacement or total hip replacement surgery will provide the best outcome for patients with hip fractures in Franklin, TN. Even in cases where patients have no evidence of osteoarthritis, various medical and anatomical considerations may make total hip replacement the more suitable treatment option. These factors include thin bone in the acetabular socket, the presence of bone cysts in the femur or pelvis, additional fractures around the hip joint, or other conditions that could compromise the success of partial hip replacement surgery. Dr. Calendine's extensive experience in both partial and total hip replacement procedures enables him to make informed recommendations based on each patient's unique anatomy, activity level, overall health status, and long-term goals. As with any orthopedic surgery, particularly hip replacement procedures, patients throughout the Nashville area are strongly advised to consult with Dr. Calendine, a board-certified, fellowship-trained orthopedic surgeon with specialized expertise in hip fracture surgery and joint replacement. During your consultation, Dr. Calendine will provide personalized recommendations based on your specific circumstances, medical history, and his extensive experience with various implants and surgical procedures to ensure you receive the most appropriate treatment for your individual situation.
Partial hip replacement animation by Understand.com
Partial hip replacement surgery removes and replaces only the ball portion of the hip joint while preserving the patient's natural hip socket. This specialized hip hemiarthroplasty procedure is most commonly performed to repair specific types of hip fractures, particularly femoral neck fractures that have disrupted blood supply to the femoral head. The hip implant used in partial hip replacement consists of a high-quality ceramic or metal ball component that is securely attached to a precisely engineered metal stem. Dr. Calendine carefully positions this metal stem down into the core of the thighbone or femur, ensuring optimal stability and function for patients throughout Middle Tennessee. If you have suffered a hip fracture or are experiencing hip pain in the Greater Nashville area, contact Dr. Calendine's practice to schedule a consultation and determine if partial hip replacement or another treatment option is right for your specific condition and recovery goals.
Source:
American Academy of Orthopaedic Surgeons, https://orthoinfo.aaos.org/; American Association of Hip and Knee Surgeons, https://hipknee.aahks.org/total-hip-replacement/; BoneSmart, https://bonesmart.org/hip/partial-hip-replacement-surgery/
Cory Calendine, MD is an Orthopedic Surgeon and founding partner of the Bone and Joint Institute of Tennessee at Williamson County Hospital in Franklin, TN. Dr. Calendine is an expert in Joint Replacement, specializing in Hip and Knee Surgery. From diagnosis through treatment, the Orthopedic Surgical experts at the Bone and Joint Institute use the latest techniques and technology to improve care for people with musculoskeletal problems. For more information, please contact our office or schedule your appointment today.