My surgeon talks about hip replacement "approach'
The surgical approach used during total hip replacement surgery refers to the direction and method by which Dr. Calendine gains access to your hip joint to perform the procedure. At our Franklin, Tennessee practice, Dr. Calendine offers patients access to various proven surgical approaches, each named according to the anatomical direction from which the hip replacement surgery is performed. The most traditional method is the posterior approach, which involves accessing the hip joint from the back of the hip and remains widely used by orthopedic surgeons across Nashville and Middle Tennessee. However, Dr. Calendine specializes in the increasingly popular anterior approach hip replacement, a minimally invasive technique that allows access to the hip joint from the front surface of the hip. The lateral approach represents a less frequently utilized option in modern total hip replacement surgery. Each hip replacement approach offers distinct advantages and considerations, and orthopedic surgeons often develop expertise and preference for specific techniques based on their specialized training, surgical experience, and patient outcomes. As Chief of Orthopaedic Surgery at Williamson Medical Center and founding partner of the Bone and Joint Institute of Tennessee, Dr. Calendine has extensive experience with anterior approach hip replacement surgery, which often provides patients with faster recovery times, reduced dislocation risk, and improved early mobility. The most important factor in achieving successful hip replacement surgery is selecting a board-certified, fellowship-trained orthopedic surgeon like Dr. Calendine who has demonstrated expertise and comfort with the chosen surgical approach, ensuring safe and precise implantation of your hip replacement components. During your consultation for hip replacement surgery in the Greater Nashville area, Dr. Calendine will discuss which surgical approach best suits your individual anatomy, lifestyle, and recovery goals.
anterior hip vs. Posterior (traditional) hip replacement
The primary difference between anterior hip replacement and posterior hip replacement lies in the location of the surgical incision, which directly determines which muscles must be cut or moved aside during your total hip replacement surgery. Dr. Calendine's expertise in anterior approach hip replacement in Nashville and Franklin, Tennessee involves making the surgical incision at the front of the hip, while more traditional hip replacement techniques utilize incisions at either the back of the hip, known as the posterior approach, or the side of the hip, called the lateral approach. Compared to posterior hip replacement surgery, anterior hip replacement typically involves significantly less damage to muscles and other soft tissues surrounding the hip joint. However, anterior approach hip replacement is considered a more technically challenging procedure that requires specialized training and experience, which Dr. Calendine has mastered as Chief of Orthopaedic Surgery at Williamson Medical Center.
Research from the prestigious Mayo Clinic in Rochester, Minnesota demonstrates that patients who undergo anterior hip replacement surgery experience objectively faster recovery compared to those who receive posterior hip replacement. According to this comprehensive study, patients who had anterior approach hip replacement in Middle Tennessee and nationwide showed improved recovery timelines in multiple key areas. Anterior hip replacement patients discontinued walker use after an average of 10 days compared to 14.5 days for posterior approach patients, stopped using all gait aids after 17.3 days versus 23.6 days, discontinued narcotic pain medications after 9.1 days compared to 14 days, were able to climb stairs with assistance after 5.4 days versus 10.3 days, and could walk six blocks after 20.5 days compared to 26 days. These significant improvements in recovery metrics demonstrate why Dr. Calendine specializes in anterior approach hip replacement for patients throughout the Greater Nashville area.
Anterior hip replacement surgery is considered less invasive than posterior or lateral approaches, though patients often associate minimally invasive surgery with smaller incisions. While anterior approach hip replacement typically uses a standard-sized incision similar to other techniques, it is frequently referred to as minimally invasive hip replacement surgery due to the significantly reduced muscle damage and cutting required. The reason anterior hip replacement performed by Dr. Calendine in Franklin, TN is considered minimally invasive relates to the preservation of critical hip muscles and soft tissues during surgery. Orthopedic experts agree that the amount of damage to muscles and other soft tissues during total hip replacement surgery represents a primary factor in recovery speed and post-surgical function. Less muscle damage during hip replacement surgery is consistently associated with faster healing, reduced pain, and improved long-term outcomes, which is why Dr. Calendine has made anterior approach hip replacement a cornerstone of his practice serving patients throughout Middle Tennessee.
location of incision and muscles affected
Anterior hip replacement surgery performed by Dr. Calendine in Nashville and Franklin, Tennessee is accomplished through a carefully planned incision that typically begins at the top of the pelvic bone, known as the iliac crest, and extends down toward the upper portion of the thigh. In some cases, Dr. Calendine may utilize a horizontal incision approach based on individual patient anatomy and surgical requirements. Once the surgical incision is made during anterior approach hip replacement, muscles are gently pushed aside rather than cut, allowing Dr. Calendine to access and visualize the hip's ball-and-socket joint while preserving critical muscle tissue. Anterior hip replacement surgery presents greater technical challenges since it requires the surgeon to work skillfully between muscles to gain optimal access to the hip joint. However, the natural anatomical separation at the front of the hip provides experienced surgeons like Dr. Calendine with ready access to the hip joint while achieving minimal or no muscle cutting, a key advantage of this muscle-sparing technique. As with all total hip replacement procedures, anterior approach surgery requires careful dislocation of the hip and precise shaping of the ball and socket joint bones to accommodate the prosthetic hip joint components using advanced surgical instruments and techniques.
The anterior approach to hip replacement surgery provides Dr. Calendine with a more limited surgical view of the hip joint compared to traditional approaches, making this procedure technically challenging and requiring extensive specialized training and experience. As Chief of Orthopaedic Surgery at Williamson Medical Center and a fellowship-trained orthopedic surgeon, Dr. Calendine has mastered the complex techniques necessary for successful anterior hip replacement surgery in Middle Tennessee. Compared to traditional posterior hip replacement, anterior approach hip replacement involves significantly less damage to the muscles and other soft tissues surrounding the hip joint, leading to faster recovery and improved patient outcomes. Even though anterior hip replacement surgery is technically more demanding for surgeons, it has become the increasingly popular choice for patients and orthopedic specialists throughout the Nashville area due to its superior recovery benefits. When considering anterior approach hip replacement surgery in Franklin, TN, it is essential to consult with a board-certified orthopedic surgeon like Dr. Calendine who possesses extensive training, experience, and proven success with anterior hip replacement techniques. Dr. Calendine's specialized expertise in minimally invasive anterior hip replacement surgery ensures optimal implant placement, muscle preservation, and the best possible outcomes for patients seeking advanced hip replacement care in the Greater Nashville region.
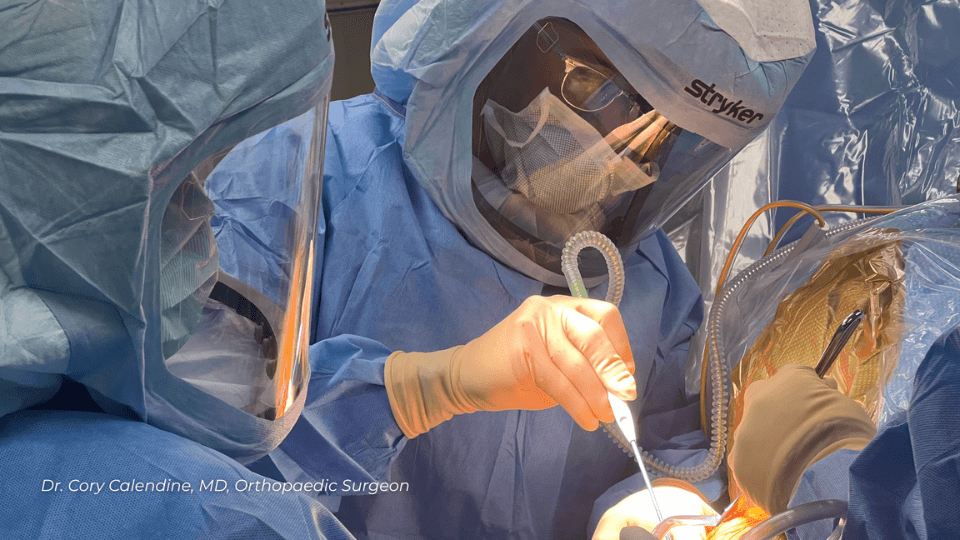
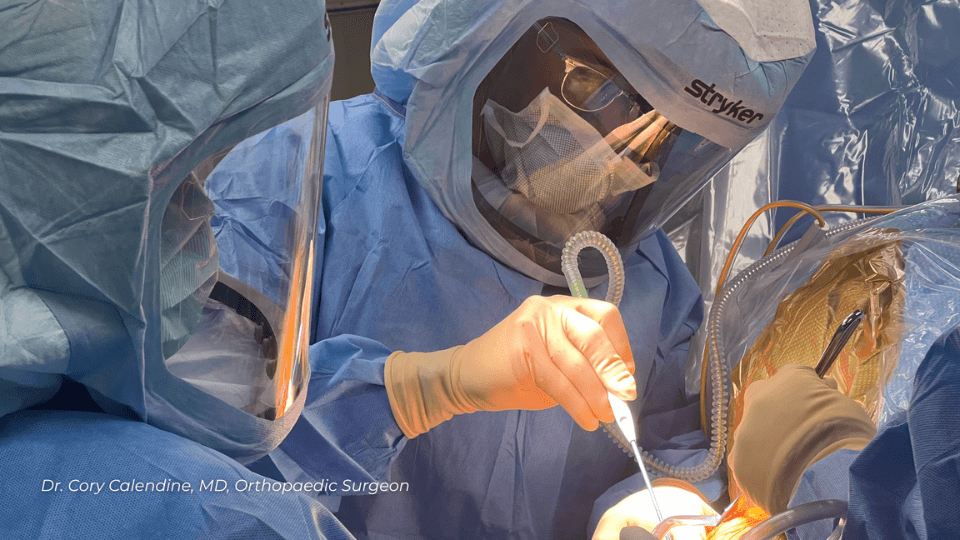
anterior hip replacement surgical procedure
During anterior approach hip replacement surgery in Nashville and Franklin, Tennessee, Dr. Calendine makes the surgical incision at the front of the hip rather than through the buttocks or side of the hip as required in traditional posterior or lateral approaches. This innovative muscle-sparing technique allows Dr. Calendine to reach the hip socket and perform total hip replacement surgery without cutting through major muscle groups that are essential for walking, balance, and daily activities. By preserving these critical muscles during anterior hip replacement surgery, patients at Williamson Medical Center and throughout Middle Tennessee often experience significantly less post-operative pain, faster recovery times, and fewer complications compared to standard hip replacement procedures. Dr. Calendine's expertise in anterior approach hip replacement surgery represents a major advancement in minimally invasive orthopedic care, offering patients in the Greater Nashville area access to this superior surgical technique that prioritizes muscle preservation and optimal healing. The anterior hip replacement approach performed by Dr. Calendine in Franklin, TN has proven particularly beneficial for active adults who want to return quickly to work, recreational activities, and independent living with minimal disruption to their lifestyle and mobility
Source:
American Academy of Orthopaedic Surgeons, https://orthoinfo.aaos.org/; American Association of Hip and Knee Surgeons, https://hipknee.aahks.org/total-hip-replacement/Cory Calendine, MD is an Orthopedic Surgeon and founding partner of the Bone and Joint Institute of Tennessee at
Williamson County Hospital in Franklin, TN. Dr. Calendine is an expert in Joint Replacement, specializing in Hip and Knee Surgery. From diagnosis through treatment, the Orthopedic Surgical experts at the Bone and Joint Institute use the latest techniques and technology to improve care for people with musculoskeletal problems. For more information, please contact our office
or schedule your appointment today.